February 10, 2023
Quality and cost variation are pervasive and plague the U.S. health care delivery system. Centers of excellence (COEs) are groups of health care providers who practice high-quality, efficient care for reasonable and predictable prices. Employers and health plans on their behalf have contracted with COE providers for 20 or more years. However, the scope of conditions and procedures offered via COEs has evolved and expanded considerably – from low-volume, high-cost procedures like transplants to far more common conditions like joint replacements and mental health. Quality and cost outcomes of many COEs appeal to employers, as they have the potential to transform the cost of health care. Therefore, employers should evaluate their benefit strategy for opportunities to steer employees to high-performing COEs.
What is a COE?
Generally, COEs are groups of providers who are selected to perform certain specialized services because of their expertise, outcomes and favorable financial arrangements. There is no standardized definition of a COE, putting the onus on employers and their industry partners (e.g., health plans, consultants) to assess the quality of COEs. According to Business Group on Health’s 2023 Large Employers’ Health Care Strategy and Plan Design Survey, the vast majority of large employers offer access to at least one type of COE in 2023 through their health plans, while some do so through a direct contract with COEs or a specialty COE network (Figure 1).
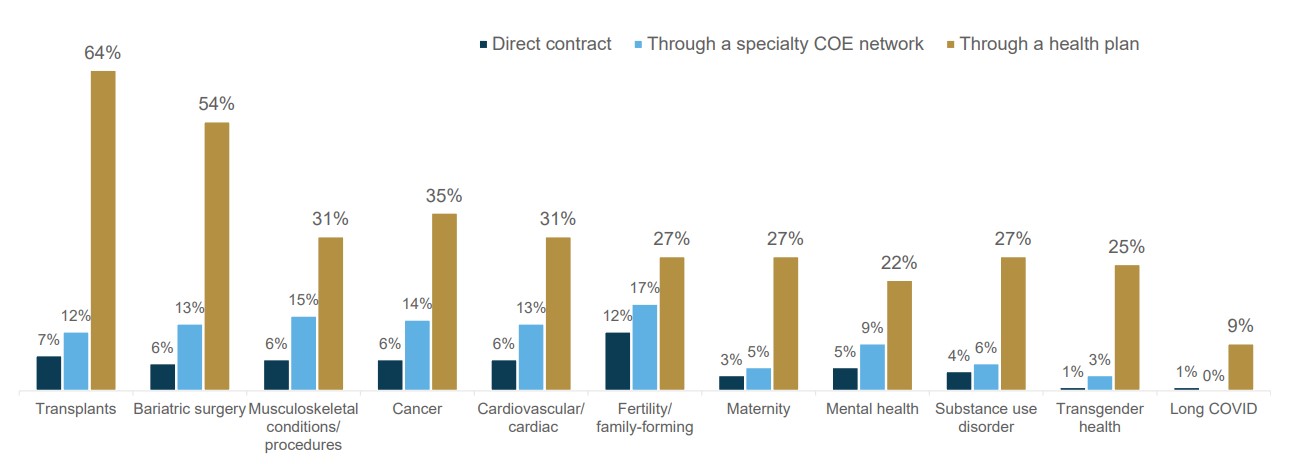
Source: 2023 Large Employers’ Health Care Strategy and Plan Design Survey
Key Takeaways
- COEs are one part of a broader value-based care strategy, which can include steerage to physician-based accountable care organizations (ACOs), high-performance networks (HPNs) and on-site/near-site clinics. Careful and coordinated integration of these models is a must. See the Business Group’s Value-based Purchasing Employer Guide for more information.
- Conditions covered by COEs have expanded over time, from low-volume, complex cases like transplants to higher-volume conditions like maternity and mental health, extending their impact.
- By 2025, a majority of employers expect to have COEs for transplants, bariatric surgery, musculoskeletal (MSK) procedures, cancer, cardiac care, fertility/family-forming, mental health and substance use disorders (SUDs).
- “Excellence” varies across COEs. Employers can assess their data to see if their current COE criteria are delivering desired results.
- COE contracts should include a second-opinion review prior to conducting procedures. Significant value is created by avoiding unnecessary surgery.
- Employers have several tools to encourage their plan members to use a COE over other in-network providers. Available tools can range from simply communicating the benefits of high-quality care and some plan design incentives for using a COE, all the way to requiring use of a COE in order to receive coverage. Most employers do not require use of a COE, except for fertility treatment and bariatric surgeries, where COEs are more common.
Which Conditions or Procedures are Covered by COEs?
COEs have traditionally covered procedures that are complex, episodic and high cost for individual patients and employers. For conditions like transplants or heart surgery, patients are more willing to change providers and/or travel for higher-quality outcomes, whereas chronic conditions like diabetes or hypertension can be adequately treated by providers in the community without patient disruption. Time-limited procedures are more easily reimbursed via bundled payments, which are incorporated into many COE contracts to ensure appropriate coordination of care back in the community and increase predictability of costs.
Emerging and Expanding Conditions or Procedures Covered by COEs
- Cancer: Large employers identify cancer as the top condition driving their health care costs in 2023, likely driving the significant interest in cancer COEs; 50% of employers offer cancer COEs in 2023, and another 26% are considering implementation in the next 2 years (Figure 2). A growing number of employers are continuing to contract with and steer employees to cancer COEs to get better patient outcomes and more value-based care arrangements. This momentum appears positioned to continue in the aftermath of the COVID-19 pandemic, which led to deferred cancer care and preventive screenings. In fact, the Business Group’s 2023 Large Employers’ Health Care Strategy and Plan Design Survey results show that 13% of employer respondents are currently seeing an impact from deferred care—an increase in late-stage cancers—while 44% anticipate seeing this impact in the near term.
- Maternity: With the continued challenge of inappropriately high C-section rates in several hospitals, as well as unacceptable rates of maternal mortality, particularly for Black women, there are opportunities for improving outcomes and reducing overall cost.1 One challenge for this type of COE is that patients may have a well-established relationship with an OB/GYN prior to conception and birth, which may make steering them to COE hospitals or partnering with providers outside their OB/GYN’s normal practice more difficult. Nevertheless, survey findings reveal that the number of large employer respondents offering COEs for maternity increased from 22% in 2022 to 31% in 2023—and this growth is poised to continue, with an additional 13% of surveyed employers considering offering COEs for maternity in 2024/2025 (Figure 2).
- Mental health: Given the prevalence and complexity of treating mental health conditions, there is a tremendous opportunity to expand COEs for SUD and other mental health issues. But there are still some challenges. For example, quality measurement in mental health care is relatively new compared to physical health. Additionally, most mental health conditions are chronic, so it may take longer to measure outcomes meaningfully than for discrete procedures.2 Even so, 55% of surveyed employers are offering or are considering offering mental health COEs in 2024/2025 (Figure 2). COEs for SUD are on the rise as well, with 34% of employers offering them in 2023 and an additional 29% considering doing so in 2024/2025 (Figure 2).
- Long COVID: Understanding and responding to long COVID is becoming increasingly important as the long-term impacts of COVID-19 become more well known. COE offerings for long COVID are increasing: In 2023, 9% of surveyed large employers will offer a long COVID COE, with another 12% considering doing so in 2024/2025 (Figure 2).
- Transgender: Another type of COE is one that provides care and services geared specifically toward meeting the health needs of transgender individuals. From a quality-assurance perspective, COEs treating individuals who are transgender and/or gender nonconforming must have a certain level of cultural competency/congruency to be considered truly effective.
For further insights and information about transgender-inclusive benefits, check out the Business Group’s A Closer Look at the Evolution of Inclusive and Equitable Transgender Benefits and Policies.
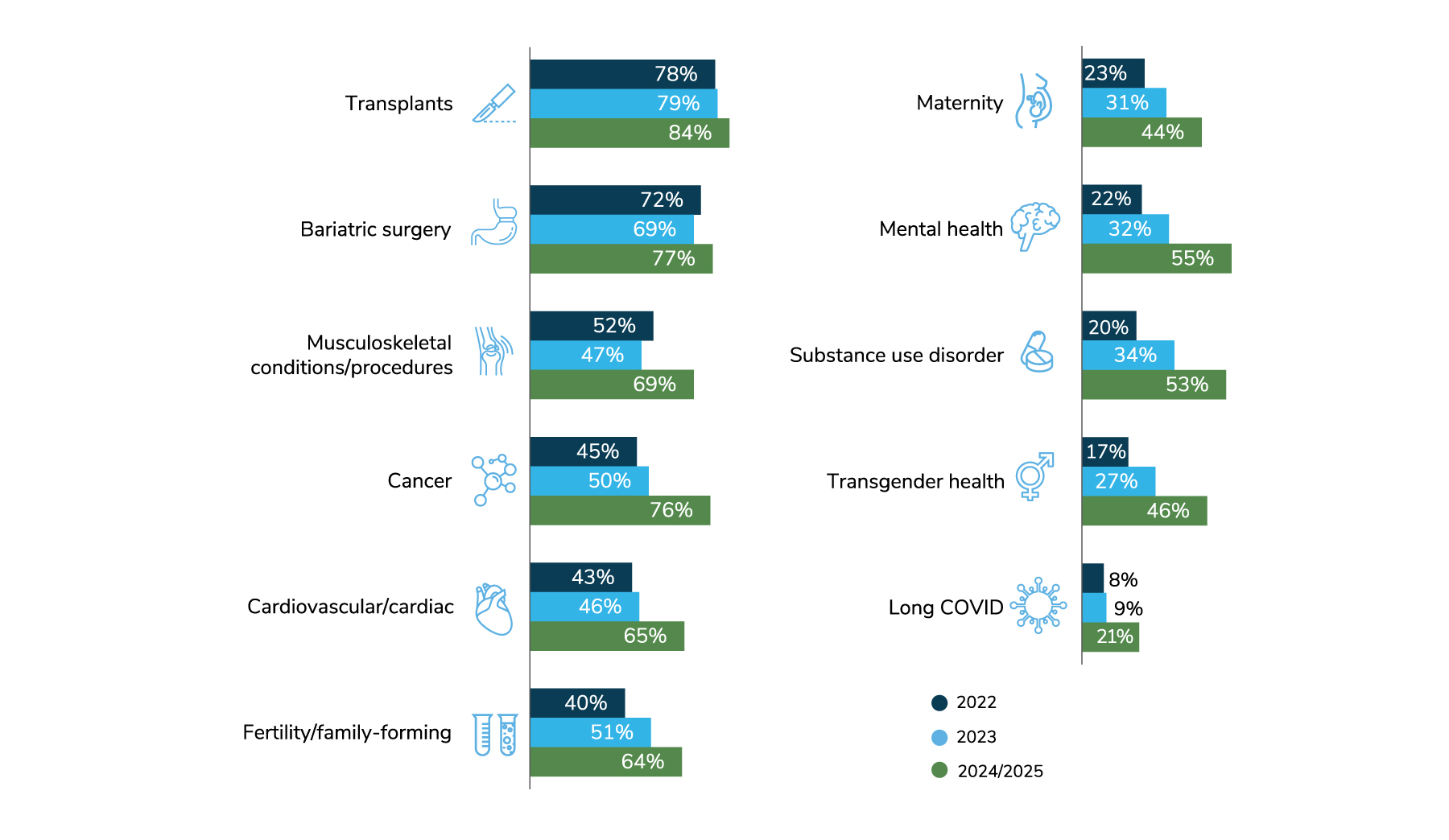
Source: 2023 Large Employers’ Health Care Strategy and Plan Design Survey
Key Questions Employers Should Ask Their Carriers About COE Strategies
- What conditions or procedures are currently part of your COE offerings, if any? How do these COEs perform compared to non-COE providers on employee population outcomes, readmission rates, time back to work, appropriate utilization, patient experience and other metrics of interest?
- Which high-cost conditions appear frequently in your employee population for which the company does not currently offer a COE? Are there significant quality, outcomes or cost variations among providers for these conditions that would warrant a COE strategy?
- Which quality metrics are of greatest importance to your company? Will you rely on health plan inclusion criteria or create your own custom COE network? How often will you reevaluate inclusion criteria and provider eligibility?
- Are you willing to create travel programs and benefits if only a handful of provider groups meet your standards? What exception criteria will you implement for those unable to travel to a provider within a given geographic distance?
For more information on steps that employers should consider for identifying high-performing COEs and promoting them for eligible plan members, see section II.
More Topics
Articles & Guides- 1 | Marill MC. Raising the stakes to advance equity in Black maternal health. Health Affairs. 2022;41(3):324-330. https://www.healthaffairs.org/doi/10.1377/hlthaff.2022.00036. Accessed December 16, 2022.
- 2 | Hazelden Betty Ford Foundation. Comparing Alcohol and Drug Rehab Success Rates. https://www.hazeldenbettyford.org/about/treatment-success-rates. Accessed December 16, 2022.
This content is for members only. Already a member?
Login
![]()
