February 26, 2024
What Are Intensive Behavioral Interventions and Who Can Benefit From Them?
Intensive behavioral interventions are the foundation of all treatments for overweight and obesity and are designed to help participants achieve or maintain a 5% or greater weight loss. Five percent or more weight loss is desired because “a 5 to 10% reduction in baseline weight is associated with clinically meaningful improvements in obesity-related metabolic risk factors and coexisting disorders”.1
Intensive behavioral interventions are conducted either in-person or electronically (or a mix of both), individually or in a group (or a mix of both) and are led by trained interventionists (i.e., health professionals or trained health educators). As the name implies, intensive behavioral interventions engage participants in behavior change strategies, such as cognitive behavioral therapy, and help them make dietary changes through nutritional counseling and increase physical activity.2,3
Employees with a body mass index (BMI) ≥30 or those with a BMI >25 with one or more cardiovascular risk factors may benefit from participation in intensive behavioral interventions.3
Why Should Employers Offer Intensive Behavioral Interventions?
Evidence shows that intensive behavioral interventions can lead to clinically significant improvement in weight status (5% weight loss) and reduced incidence of type 2 diabetes in people with obesity.3 Some studies also show that intensive behavioral interventions can significantly improve quality of life measures, including self-reported quality of life, physical functioning, self-esteem and work and daily activities, compared to usual care.4
Experts recommend that providers screen patients annually for obesity using BMI and/or waist circumference and that they report these results back to the patient’s primary care physician if done by another professional.3,5 Screening enables providers to refer people with obesity to intensive behavioral interventions and a diagnosis of obesity can be a driver of weight loss success.6 It’s important to note that in 2023, the American Medical Association declared the use of BMI on its own an “imperfect clinical measure” because it fails to distinguish between fat and lean tissue. Additionally, because individuals with the same BMI can have different health profiles, BMI is an inadequate sole indicator of overall health and risk factors.7 Combining BMI with waist circumference is a preferred measurement approach because it provides a more comprehensive assessment of body composition and health risks.8
What Are the Components of Effective Behavioral Interventions?
People who participate in high-intensity behavioral interventions generally lose more weight and have greater reductions in waist circumference than those in low- to moderate-intensity interventions.3 Research indicates that the benefits of intensive behavioral interventions may depend on the following factors:
- Number of sessions (i.e., intensity): A higher number of sessions is associated with more weight loss.3 For example, a research review found that high-intensity interventions (12-26 sessions per year) average 6% weight loss, whereas those in low- to moderate-intensity programs (<12 sessions per year) average 2.8% weight loss.9 A study published in 2020 had similar results: The average percentage weight loss among those who participated in a high-intensity intervention was 4.99% at 24 months, compared to .48% average weight loss among those who received usual care.4 Participants in the high-intensity intervention had weekly sessions for the first 6 months, followed by monthly sessions for the remaining 18 months. Those in the usual care group received standard care from their primary care team.4
- Peer support: The inclusion of group sessions – either as the main mode of delivery or as an additional component – is related to greater weight loss.3
- Personalization: The benefits of behavior-based interventions may depend on the ability to tailor it to the social, environmental and individual factors of the employee.3 These factors may include things like income, health literacy and culture, as well as preferences and needs.
- Delivery: In-person and virtual programs may be similarly effective in terms of short-term weight loss and dropout rates, according to a 2020 study.10
Are Intensive Behavioral Interventions Offered in the Primary Care Setting?
Although policies and practice guidelines have laid the groundwork for physicians to play a greater role in delivering behavioral interventions in the health care setting, nearly two-thirds of surveyed physicians have said they lack effective strategies to help patients with overweight or obesity.11 Even when weight-related counseling or guidance does take place in the physician’s office, patient-provider interaction is typically not frequent enough to be considered a high-intensity intervention.
To successfully deliver behavioral interventions in the primary care setting, different models of care may be necessary. For example, intensive behavioral interventions have been successfully delivered in primary care when trained health coaches were embedded in the care team.4 And while more research is needed to explore their effectiveness for obesity treatment, shared medical appointments (where multiple people with the same diagnosis receive care from a multidisciplinary team in group sessions) may have potential in primary care or other health care settings.10,12 These sessions may include the components that evidence indicates is necessary for weight loss.10,12
What Type of Behavioral Interventions Do Employers Offer?
According to the 14th Annual Employer-Sponsored Health and Well-being Survey, 74% of employers have a weight management program in place in 2023; 89% are considering for 2024.13 A separate Business Group on Health survey found that 58% of employer respondents offered virtual health services for traditional weight management focused on behavior change in 2023 and another 4% are adding them in 2024.14 Twenty-two percent of employers offered virtual medication-assisted weight management in 2023, with an additional 4% adding them in 2024.14 Such virtual programs allow employers to offer scalable interventions.15
Other programs that employers have offered include telephonic disease management or coaching, group-based weight management (either on-site or in the community), meal replacement programs (which may be offered alongside behavioral interventions) and medically supervised weight management.15 While not all of these programs are intensive behavioral interventions, some may include the elements that evidence indicates are necessary to achieve at least 5% weight loss.
Employer Example: Medical Weight Loss
One employer has brought medical weight loss virtually to all states and two on-site primary care clinics at their employee clinic locations. The internally developed program integrates behavioral counseling by clinicians, including physicians, advance practice clinicians (APC), registered nurses and registered dietitians who have been clinically trained in obesity treatment with pharmacotherapy for patients who qualify. The medical weight loss program begins with an intake assessment and labs followed by a 60-minute consultation with a physician or APC who develops an individualized care plan. After that, employees and the physician or APC and coach (registered dietitian) meet at least once every 3 months for the first year and at least bi-annually thereafter. In between these meetings, participants are able to connect with their provider or registered dietitian via messaging at any time. These services are covered on an eligible medical plan for employees who meet the criteria for participation. Among those who have taken part in the medical weight loss program, 62% have lost clinically significant weight loss (defined as 5% or greater of their body weight) at the 6-month mark, and greater than 70% have sustained greater than 5% weight loss beyond 12 months. Demand for medical weight loss is high with approximately 3,500 interest form completions in the last 3 months.
Do Employers Provide Incentives for Weight Management and Are They Effective?
Prevalence
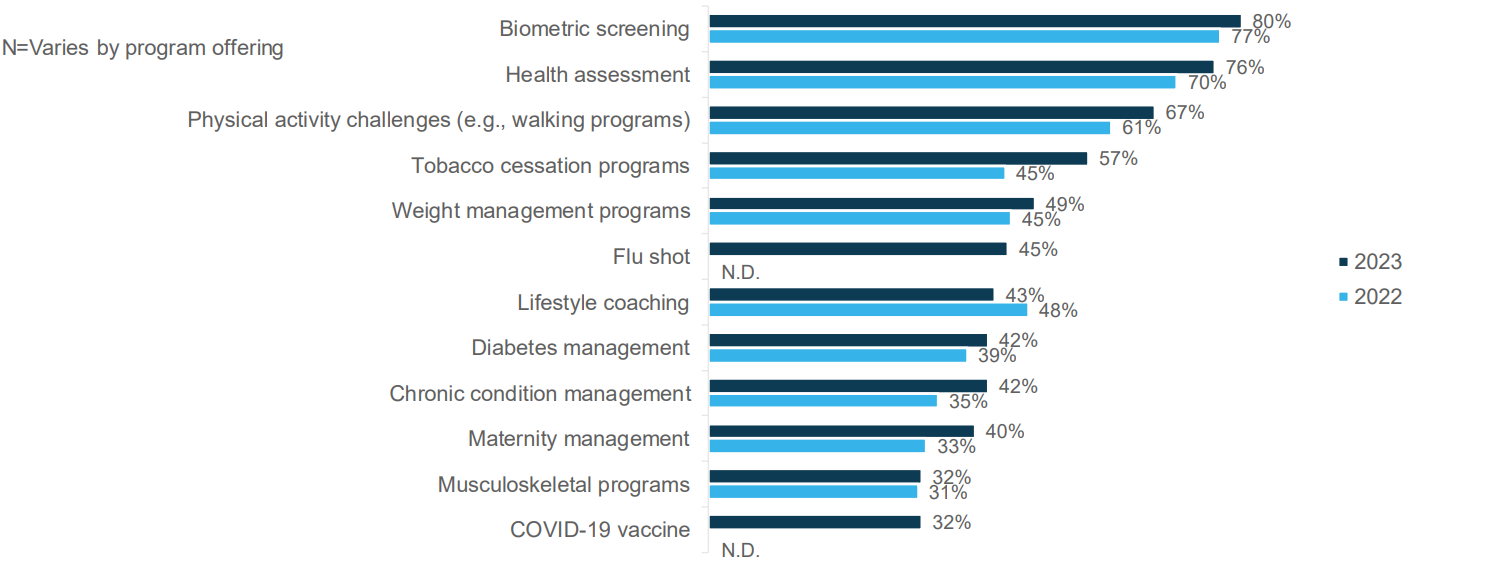
Among surveyed employers with weight management programs, 49% offer incentives to employees to participate in these initiatives in 2023, an increase from 45% in 2022 (see Figure 2.1).13 The use of outcomes-based incentives continued to decrease in recent years with 12% of surveyed employers using this type of incentive in 2023.13
Effectiveness
There is evidence that various types of financial incentives may promote initial weight loss among those who receive them.16-19 However, this isn’t consistent across all studies; for example, an 18-month long study published in 2021 found that employees who received a daily lottery prize if they met their weight goal did not achieve significantly greater weight loss than those who did not receive incentives, and the results were similar 6 months later.20 Research also indicates that even when incentives promote weight loss, it is not sustained over time.16-19
A small study examining the attitudes of adults about the acceptability and usefulness of incentives for weight loss maintenance helps explain why incentives may not be useful for weight loss. The study found low support for any type of incentives among adults with overweight and obesity who had completed a weight management program, and particularly for deposit contracts and lotteries.21 More appealing to this population were ongoing weight management programs and peer support.21
What Questions Should Employers Ask When Designing and Implementing Intensive Behavioral Interventions?
- Do current or prospective weight management programs include the components that evidence indicates are necessary for weight loss? Whether they’re developed internally or vendor run, ensure that interventions incorporate behavior change strategies and address nutrition and physical activity. Physical activity, including resistance training, is particularly important because weight loss (regardless of how its accomplished) can also lead to loss of muscle mass.22 Beyond the aforementioned critical components, it may be helpful for interventions to address other factors important to weight loss, including sleep, stress management and mental health support. Interventions should be high-intensity and include peer support and personalization.
- Do current or prospective weight management programs include weight loss maintenance strategies? Beyond targeting weight loss, interventions should have maintenance and/or relapse prevention strategies. This may include at least monthly sessions for 1 year or more that have ongoing behavioral therapy and guidance on nutrition and physical activity.5 While crucial for all patients, maintenance strategies are especially important for individuals who discontinue the use of anti-obesity medications in order to mitigate weight regain.
- Do weight management program practitioners have appropriate training and credentials? Providers engaging patients in behavioral strategies should be trained in behavior change techniques such as cognitive behavioral therapy or motivational interviewing. Providers working with patients on their dietary strategy should have expertise in nutrition; these professionals could be a registered dietician, nutritionist or other clinician with expertise in this field. Similarly, providers working with patients on increasing physical activity and mobility should have appropriate credentials (e.g., exercise physiologist, certified personal trainer). It may also be beneficial to train all weight management program providers about the other employer-sponsored benefits and programs available to employees, such as mental health and nutrition, and to refer employees when appropriate.
- Are weight management programs relevant to the target population? Employee data and input obtained through focus groups or surveys can increase the odds the program resonates with employees. For example, one intensive behavioral intervention in the primary care setting adapted its intervention approaches and program materials to meet the needs of the target audience - racially diverse, low-income populations across Louisiana - by working with health literacy experts, conducting focus groups and engaging with a patient advisory board.4 Stock photos, which didn’t represent the patient population, were swapped out, language was simplified and food recommendations were adapted to reflect the local culture.23
- Do your weight management programs include the ability for clinicians to prescribe FDA approved anti-obesity medications for patients who meet criteria? As outlined in the Anti-obesity Medications section of this resource, pairing intensive behavioral interventions with FDA (U.S. Food & Drug Administration)-approved anti-obesity medications increases the likelihood that patients with obesity will achieve clinically meaningful weight loss. Some employers provide coverage of anti-obesity medications as an adjunct to behavioral interventions in on-site clinics, and some virtual weight management programs now offer anti-obesity medications as a part of their care models.
- 1 | Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. New England Journal of Medicine. 2017;376(3):254-266.
- 2 | Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults. Circulation. 2014;129(25)(2):S102–S138
- 3 | LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O'Connor EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;320(11):1172-1191.
- 4 | Katzmarzyk PT, Martin CK, Newton RL, et al. Weight loss in underserved patients — a cluster-randomized trial. New England Journal of Medicine. 2020;383(10):909-918. doi:10.1056/NEJMoa2007448
- 5 | STOP Obesity Alliance. Developing a Comprehensive Benefit for Outcomes-based Obesity Treatment in Adults. https://stop.publichealth.gwu.edu/sites/g/files/zaxdzs4356/files/2022-02/comprehensive_obesity_care_v._9.1.21.pdf. Accessed July 28, 2022.
- 6 | Kaplan LM, Golden A, Jinnett K, al. e. Perceptions of barriers to effective obesity care: Results from the national ACTION study. Obesity. 2018;26(1):61-69.
- 7 | Katella K. Why you shouldn’t rely on BMI alone. Yale Medicine. August 4, 2023. https://www.yalemedicine.org/news/why-you-shouldnt-rely-on-bmi-alone. Accessed October 17, 2023.
- 8 | Nordqvist C. Why BMI is inaccurate and misleading. Medical News Today. January 20, 2022. https://www.medicalnewstoday.com/articles/265215. Accessed January 17, 2024.
- 9 | Virginia A. Moyer, on behalf of the U.S. Preventive Services Task Force. Screening for and management of obesity in Adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012; 157(5):373-378. (5):373-378.
- 10 | Shibuya K, Ji X, Pfoh ER, et al. Association between shared medical appointments and weight loss outcomes and anti-obesity medication use in patients with obesity. Obes Sci Pract. 2020;6(3):247-254.
- 11 | Steeves JA, Liu B, Willis G, Lee R, Smith AW. Physicians' personal beliefs about weight-related care and their associations with care delivery: The U.S. National Survey of Energy Balance Related Care among Primary Care Physicians. Obes Res Clin Pract. May-Jun 2015;9(3):243-55. doi:10.1016/j.orcp.2014.08.002
- 12 | Walker R, Ramasamy V, Sturgiss E, Dunbar J, Boyle J. Shared medical appointments for weight loss: a systematic review. Family Practice. 2021;doi:10.1093/fampra/cmab105
- 13 | Business Group on Health and Fidelity Workplace Consulting. 14th Annual Employer-Sponsored Health and Well-being Survey. May 2023. https://www.businessgrouphealth.org/resources/14th-annual-health-and-well-being-survey-2023. Accessed September 26, 2023.
- 14 | Business Group on Health. 2024 Large Employer Health Care Strategy Survey. https://www.businessgrouphealth.org/resources/2024-large-employer-health-care-strategy-survey-intro. Accessed September 20, 2023.
- 15 | Business Group on Health. Quick Survey Findings: Weight Management Benefit Programs. October 2021. https://www.businessgrouphealth.org/resources/quick-survey-findings-weight-management-benefit-programs. Accessed March 4, 2022.
- 16 | John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, Volpp KG. Financial incentives for extended weight loss: a randomized, controlled trial. J Gen Intern Med. 2011;26(6):621-626.
- 17 | Kullgren JT, Troxel AB, Loewenstein G, et al. Individual- versus group-based financial incentives for weight loss: a randomized, controlled trial. Ann Intern Med. 2013 Apr 2;158(7):505-14.
- 18 | Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;10(300):2631-7.
- 19 | Yancy Jr WS, Shaw PA, Wesby L, et al. Financial incentive strategies for maintenance of weight loss: results from an internet-based randomized controlled trial. Nutrition & Diabetes. 2018/05/25 2018;8(1):33.
- 20 | Glanz K, Shaw PA, Kwong PL, et al. Effect of financial incentives and environmental strategies on weight loss in the healthy weight study: A randomized clinical trial. JAMA Network Open. 2021;4(9):e2124132-e2124132. doi:10.1001/jamanetworkopen.2021.24132
- 21 | McGill B, O’Hara BJ, Grunseit AC, et al. Acceptability of financial incentives for maintenance of weight loss in mid-older adults: a mixed methods study. BMC Public Health. 2018/02/13 2018;18(1):244.
- 22 | Blum D. The risks of taking drugs like Ozempic when you’re Over 65. The New York Times. https://www.nytimes.com/2023/07/17/well/ozempic-wegovy-risks-older.html. Accessed December 3, 2023.
- 23 | National Alliance of Healthcare Purchaser Coalitions. Rethinking how employers support the obesity patient journey webinar. December 14, 2021. https://connect.nationalalliancehealth.org/viewdocument/rethinking-how-employers-support-th. Accessed March 24, 2022.
More Topics
Articles & Guides-
Part 1An Employer's Practical Playbook for Treating Obesity
-
Executive SummaryRaising the Bar: 6 Ways Employers Can Elevate Their Weight Management Strategy
-
Part 2Intensive Behavioral Interventions
-
Part 3Anti-obesity Medications
-
Part 4Bariatric Surgery
-
Part 5Workplace Culture and Design
-
Part 6Appendix
This content is for members only. Already a member?
Login
![]()
