February 20, 2023
The Health Innovations Forum (HIF), a group of leading Business Group on Health members, is unique in that it not only identifies, but also accelerates the adoption of effective innovations in health and well-being strategies. One of many ways HIF members do this is by assessing innovative start-ups and growing companies looking to partner with self-insured employers to deliver transformative health benefits. Over the course of 8 years, HIF members have vetted over 100 companies, many of which have proceeded to successfully implement their solutions across a number of Business Group members and launch their companies more broadly into the employer market.
As technology and the ability to effectively utilize vast amounts of health care data have expanded, emerging start-ups and innovators have been able to target specific portions of the health care ecosystem for optimal results. But there’s a potential downside to the large number of innovators. As the focus of many innovators has turned to specific slices of the health care experience or patient populations, employers have been left wondering, “Where does this solution fit into my benefits strategy as a whole?”
The following sections take a close look at issues employers should consider as they strive to build a cohesive benefits strategy that includes desired innovations.
The Challenge of Optimizing One Piece of the Puzzle
Self-insured employers work with a multitude of vendors to deliver their health and well-being benefits. At its most benign, implementing a new strategy or solution that optimizes only a small niche of the health care ecosystem may be a headache for some benefits leaders, who need to navigate their finance, legal, IT, and procurement teams for any solution, whether for a large or small group of plan members. At worst, a niche solution – even one that is effective at reaching its intended goal – may create confusion for employees and further fragment an already disjointed ecosystem by disrupting existing positive relationships with health care providers and vendor programs. The accelerating adoption of virtual health solutions has further exacerbated these preexisting challenges and emphasized the need for employers to partner with vendors who seek to holistically address and ameliorate these poignant pain points. When surveyed, most large employers were aware of the potential pitfalls of too many vendors and noted that employees could have a siloed experience due to lack of coordination between virtual and community-based providers and lack of integration between vendors (Figure 1).
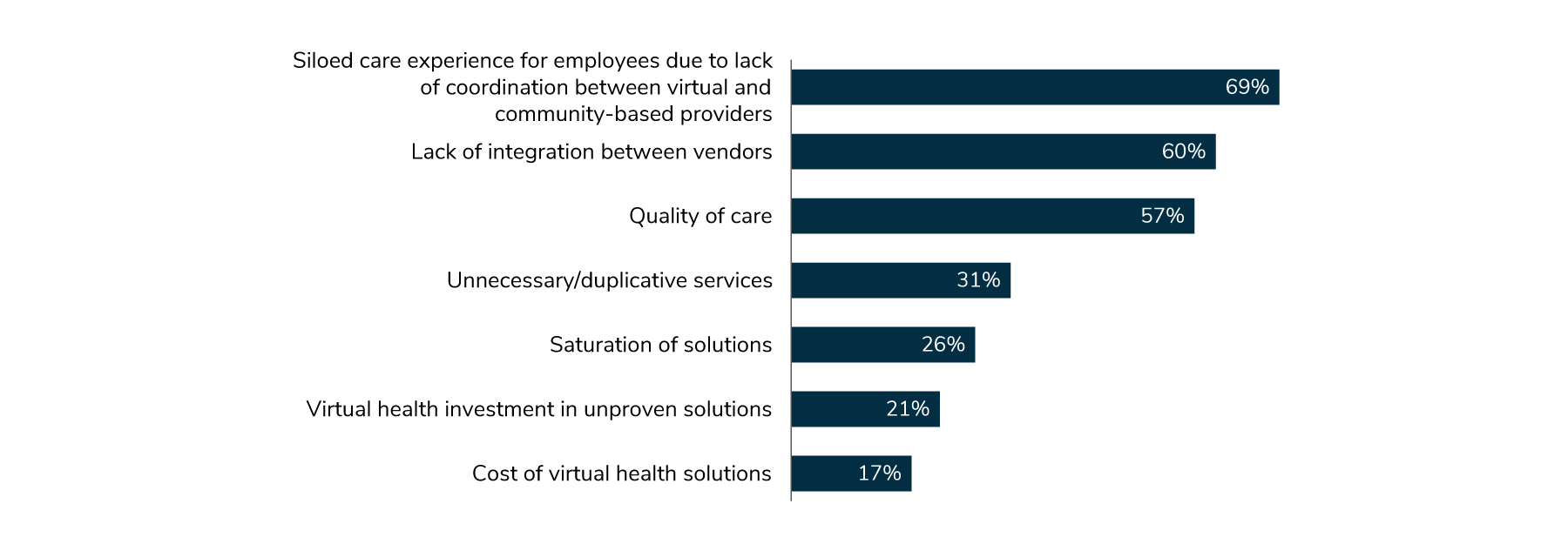
Source: From 2023 Large Employers’ Health Care Strategy and Plan Design Survey. Business Group on Health
In some cases, vendors looking to partner directly with large employers may have more success contracting with health plans, health care providers, aggregators or other established industry players. These stakeholders may be better positioned to integrate the solution into their coordinated services for plan members.
Evolution of Innovation in Health Care
HIF was created in 2015 to assist employers in assessing the vast number of emerging start-up solutions, understanding the gaps those solutions could fill and ultimately what benefit those solutions might bring to an employer’s overall health and well-being strategy. To date, over 300 companies have applied, and a significant subset of those have presented their solutions to Forum members. Many of these presenting companies have gone on to great success in the employer market.
But for large employers, innovation isn’t just partnering with exciting start-up companies. Employers increasingly express “point solution fatigue” from contracting with too many vendors, compounded by the fact that none are truly integrated with each other. The process of incorporating vendors across procurement, legal, IT, communication, and other departments can be onerous, and integrating a new solution into the employer’s existing vendor ecosystem is a major headwind. Responding to this dynamic, HIF continues to vet start-up companies but also takes a more holistic view of accelerating the adoption of innovative strategies and partnerships. The group has facilitated design-thinking exercises on key topics and themes in health care, starting with primary care, to identify priorities and opportunities for effective implementation.
Recognizing that success requires collaboration, HIF includes voices from industry partners who are necessary for integrating and delivering benefits on behalf of large employers. This cross-industry collaboration is unique to HIF, but more importantly, it enables the group to explore how to seamlessly integrate vendors into the consumer and employer experience. A solution on its own may be compelling but will not have long-term impact or viability if it isn’t integrated effectively within the broader ecosystem and benefit strategy, alongside employers’ other partners and vendor solutions.

Drive change with the Health Innovations Forum.
Learn More ![]()
Effective Innovation in Primary Care is Integrated
The challenge of integration is particularly acute in primary care, which is ripe with opportunity and is a common target for innovation. Traditional primary care has fallen victim to a fee-for-service (FFS) reimbursement model that marginalizes the consumer experience, frustrates providers and limits innovation. Traditional primary care, however, remains the most common touchpoint with the health care system aside from the pharmacy counter. Ideally, primary care is a refuge for patients in what is often a fragmented, confusing and expensive health care system. A key competency of an effective primary care system is that it coordinates care for patients, guiding them through their journey within the primary care provider (PCP) office and beyond.
The breadth of the primary care experience means that some elements are often targeted by emerging vendor partners for improvement. This approach, however, isn‘t always the optimal solution. When slices of primary care are carved out, it can hamper providers’ ability to coordinate care, deliver effective preventive services and support their patients holistically with services for both physical and mental health conditions. This isn’t to say that the status quo of FFS primary care is acceptable or without substantial room for improvement, but it behooves employers to give additional scrutiny to vendors looking to optimize only one part of the primary care whole.
We Need to Optimize Primary Care, Not Just Elements of Primary Care
Across the country, there are examples of primary care arrangements that are succeeding at delivering high-quality care at a total cost better than the market. Almost without exception, these arrangements accept some risk for outcomes and total costs, or have moved away from FFS reimbursement altogether and toward a value-based delivery model. Once FFS incentives have been blunted or removed, a primary care provider and their team are free to innovate and practice in ways that optimize population health and coordination across other provider groups, embracing many of the vendor solutions referenced above while improving their bottom line.
No one vendor, provider group or employer will be able to solve the challenges of primary care alone. When incentives are aligned, data shared and patients empowered, there are tremendous opportunities to improve the primary care experience across the board, including by establishing ways for traditional providers, virtual care vendors and other point solutions to work in concert to improve the lives of the people they serve.
Taking a Step Back: Identifying Primary Care "Nirvana"
Recognizing these challenges, HIF members paused to consider what an optimal primary care experience would look like for patients. By coming to consensus on what primary care “nirvana” could be, they reasoned that they could work backward to better assess whether a new plan design, network or vendor strategy will help advance the cause of promoting this ideal state.
There are several academics and primary care-focused organizations that have created their own frameworks of what high-quality primary care looks like. However, this HIF-led process of identifying challenges and a vision for an optimal primary care experience is the most holistic look at the topic from multistakeholder representatives across the health care ecosystem, including employers, the ultimate purchasers of health services, alongside their employees and dependents.

