June 08, 2020
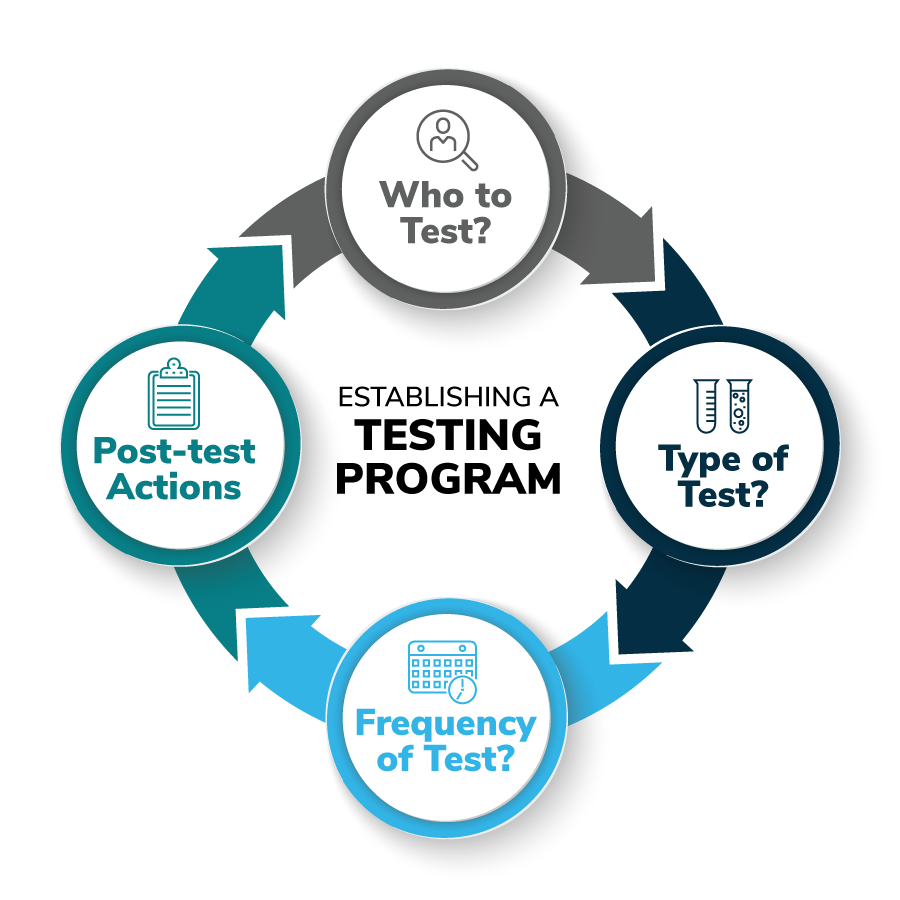
According to health experts, a community’s testing plan is pivotal to controlling the spread of the virus in the absence of an effective vaccine. The above figure shows some of the issues that need to be considered when setting up a testing program, Research by Harvard Global Health Institute suggests that a certain level of testing is needed in order for countries, states and communities to reopen safely.
According to the World Health Organization (WHO), the maximum positive rate recommended is 10%. If a community’s positive result rate is higher than that, expanded testing is needed. In mid-April, the positive rate in the US was 20%; in Germany, that number was 7%, and in South Korea, it was closer to 3%. Around the world, countries, states and local communities are focused on their testing capacity and plan. According to the COVID Tracking Project, as of late May, the positive test rate in the US had fallen to just over 10%.
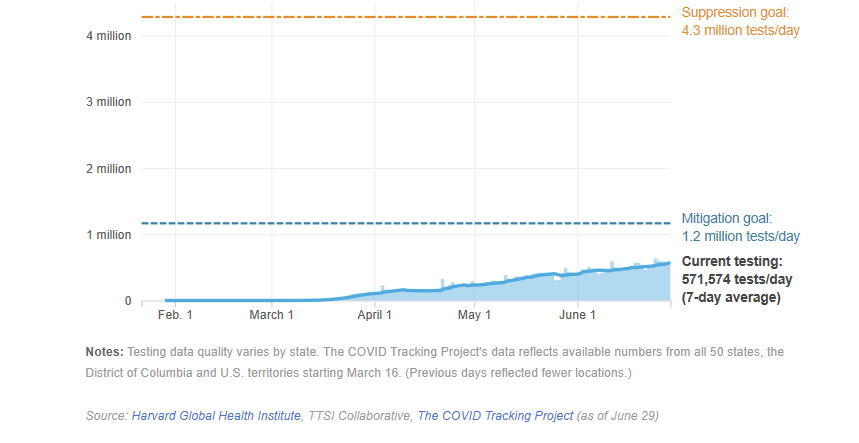
Figure 1 shows the significant increase of testing that is recommended in order for the U.S. to reopen safely, according to Harvard University researchers.
Availability of testing has been an issue In the US, and it varies by state. Some states have reported a shortage of capacity or materials, while others have indicated that they have more testing capacity than demand. Initially, to address supply and demand needs, the guidelines were designed to provide testing only to those who meet certain criteria, such as a referral by a clinician because of COVID suspected symptoms, known contact with someone who tested positive or vulnerabilities such as preexisting health conditions or age that make individuals more susceptible to infection. In some geographies, however this is starting to change. For example, Switzerland has begun to expand testing beyond only those patients showing severe symptoms; Finland announced in April that it would double testing capacity to strengthen coronavirus coordination, and the states of Georgia and New York in the U.S. are now encouraging asymptomatic testing.
Does the Employer Have a Role in Testing?
As companies bring employees back to the workplace, providing a safe and healthy environment should be their primary focus. While there is a known correlation between testing and risk mitigation, testing is not consistently available across geographies. In this highly fluid situation, testing knowledge, attitudes, availability and strategies are certain to evolve considerably over time.
As of mid-July 2020, some employers are considering providing or facilitating their own testing as part of their RTW strategy. Most employers have taken a company-wide approach to their pandemic response plan, meaning that their overall strategy, protocols and implementation are applied across locations (across states and across countries), with local tweaks made where required to account for differing local requirements, laws and disease curve stage.
Given these variables, the element of the global pandemic response plan that varies by location is the approach to testing, largely driven by differences in country health systems and local laws. As of mid-May, according to the international law firm Littler Mendelson P.C., in most countries, there are no specific laws regarding employer testing for a viral infection or antibodies. Although these local regulations are constantly evolving, at this point, they suggest that employer testing is permissible if data privacy is adhered to and qualified medical professionals administer the test.
The following list, organized by location, identifies some issues that need to be considered when thinking about testing in the workplace:
- U.S.: The Equal Employment Opportunity Commission (EEOC) updated its guidance on April 23 on the Americans with Disabilities Act (ADA) and coronavirus, explaining that employers may screen employees for COVID-19. Any mandatory medical test must be job-related and consistent with business necessity, the EEOC explained. "Applying this standard to the current circumstances of the COVID-19 pandemic, employers may take steps to determine if employees entering the workplace have COVID-19 because an individual with the virus will pose a direct threat to the health of others," the agency stated. Consequently, an employer may administer COVID-19 testing to employees before they enter the workplace. In June, following the CDC’s Interim Guidelines that antibody test results “should not be used to make decisions about returning persons to the workplace,” the EEOC stated that an antibody test at this time does not meet the ADA’s “job related and consistent with business necessity” standard for medical examinations or inquiries for current employees. Therefore, requiring antibody testing before allowing employees to re-enter the workplace is not allowed under the ADA.
- Poland: Companies would need authorization from the Chief Sanitary Inspectorate, have a Collective Labor Agreement and provide the employee with sufficient notice.
- Australia: If the company has a modern award for mandatory industrial standard, then it will have to consult with employees before implementing a testing program.
- Peru: As of mid-May, it is the only country with a law. A recent law suggests that employers must administer a test to specific categories of people (those with positive diagnosis and medically discharged, vulnerable, etc.).
- Denmark: The Ministry of Employment said employers are not allowed to require testing unless the workplace is a high-risk environment like a hospital or retirement home.
Taking into consideration any local laws that may put requirements or limitations on the employers’ role in testing, employers need to decide which approach they will take on the following questions:
- What role will the company play in testing?
- Which test(s) will be part of the plan?
- Who will be included in the testing plan?
- What actions should be taken based on test results?
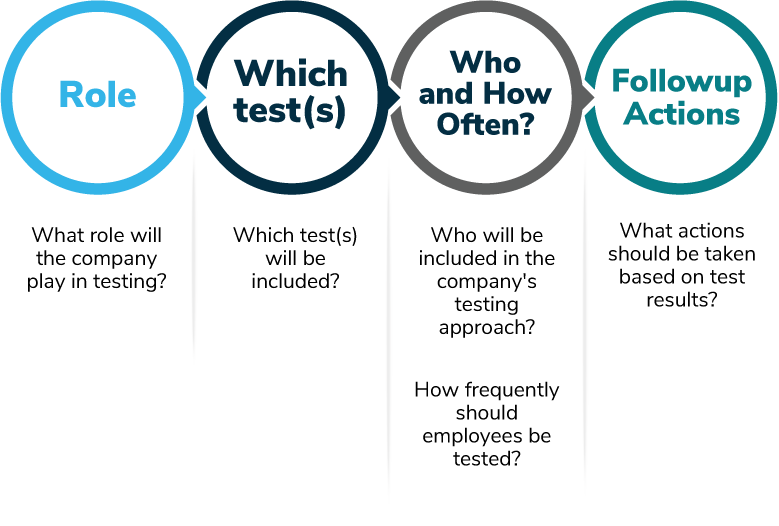
The following section provides more information about how to answer the questions raised above.
Determining the Company's Role
There are two main roles a company can decide to take:
- 1 | Rely on the health system to refer, facilitate and administer testing (understanding that such testing will only be available for individuals that meet local testing criteria).
- 2 | Take on the role of facilitating employee testing. Testing criteria and frequency can be determined by the RTW protocol and business necessity.
The below table shows the advantages and challenges of each approach.
|
|
Rely on the Health System - Activity Limited to Screening |
Company-facilitated Testing |
|---|---|---|
|
Advantages |
Decreases the need to navigate varying laws and requirements related to the employers’ role in testing. |
Increases testing rate and speed to better mitigate risk. |
|
Challenges |
Significant variability in access and capacity by location (across states in the U.S. and across countries). |
Level of risk mitigation varies depending on who is tested and frequency of testing. Limited mitigation within employers’ control; the larger community in which employees live are not subject to the enhanced testing. Privacy requirements. Consent requirements/ mandatory vs. voluntary. Other concerns: In some countries (such as Mexico), employers have decided not to facilitate testing because a positive result could mean that the employee is eligible for workers’ compensation regardless of where the employee became exposed. To avoid this possibility, one employer has chosen to leverage the health system. |
|
Examples |
In the US, some employers have decided that they will not take an active role in testing and instead refer only symptomatic employees to their physician to be tested through the health system channels. In the U.K., as part of its plan to increase testing, employers can now register by email and refer self- isolating staff to book a test online. In China, as testing becomes more accessible across the country, many companies are arranging for their staff to get tested before they resume work |
Employers in the health care industry, essential production facilities or the transportation industry have been more likely to implement on-site testing |
Approaches Vary by Company
The dynamics and needs of each employer vary. Therefore the “right” answer for approach will vary by company.
Industry, level of risk and consumer exposure will play a large role in each employers’ decision- making process about which approach makes the most sense for them.
For example, companies that have customer- facing operations and more difficulties maintaining physical distancing may be more likely to opt for an active role in testing their employees.
Which Test? The Many Varieties of Tests
For employers that decide to take an active role in testing, decisions need to be made regarding the type of test that will use. In fact, employers often discuss the importance of testing, but they are less clear about the type of test they’re considering. Options include PCR tests, antigen tests, antibody tests, home kits or other. While some employers also refer to temperature checks and Symptom Checkers as testing, for this section testing refers to viral detection or antibody tests.
Some of the tests listed above have different purposes. For example, some test for the presence of the virus, while others test for past exposure. The collection method is also different, so too are the benefits and challenges. Table 2 outlines the three main categories of tests and how they differ.
| PCR (Polymerase Chain Reaction) | Antibody Test (IgM/IgC) | Rapid Antigen Test | |
|---|---|---|---|
|
Collection Method |
Swab of nose or throat |
Serology/blood test |
Swab of nose or throat |
|
How it Works |
Detects presence of virus, current infection or virus shedding Accuracy of result depends on sample collection quality and disease state at time of test. Home kit viability as PCR test has 5- day stability. |
Detects immune response to COVID-19 infection IgM – detectable 1 week into infection. Identifies and destroys virus. Decreases over a few weeks IgG – detectable 2-3 weeks into infection. Replaces IgM. Potential for longer- term immunity |
Detects presence of virus, current infection or virus shedding Results available in 10 minutes without a lab |
|
Challenges |
Results only relevant for a point in time, as employees can be infected at any time after testing. False negatives: They can result from:
Sample sent to lab: Delay in results, dependent on availability of test supplies at lab |
Evidence of immunity is inconclusive
False positive
Does not confirm active infection * Cost considerations for large- scale testing |
Results only relevant for a point in time, as employees can be infected at any time after testing. False negatives Availability: Currently only offered to health workers and first responders |
|
Highlights |
False negatives may miss positive cases *Costly Wait for results Best for detecting active cases |
False sense of protection could promote risk
*Costly Currently may not be applicable for RTW protocols |
Future potential solution when it becomes more widely available and accurate Expected to be less costly Fast results Best for future consideration of testing customers (such as airline passengers, patients undergoing elective medical and dental procedures) |
*Note – Cost varies significantly by country and supplier and is expected to evolve and change. Various suppliers are producing tests, and availability in the marketplace depends on geography. For example, in the U.S., the Food and Drug Administration (FDA) has worked with more than 400 test developers who have already submitted or said they will be submitting Emergency Use Authorization (EUA) requests to the FDA for tests that detect the virus or antibodies to the virus. As of late May, the FDA has authorized 113 tests under EUAs, which include 1 molecular test, 12 antibody tests and 1 antigen test. Companies and employees should be aware of the potential for patients to receive surprise bills for out-of-network coronavirus testing. This possibility was made evident from preliminary findings of an investigation by the House Energy and Commerce Committee. The investigation was prompted by reports of patients receiving bills between $300 and $6,000, which far exceeds the Medicare payment of $100 per test. While the CARES Act included language that testing should be at no cost to patients, and requiring that providers list the cash price on their website, it did not limit charges if the testing is done out of network, nor did it prohibit labs or hospitals from billing patients if insurers refuse to pay their posted charges. Employers may want to work with their health plans to identify any potential out of network testing claims early and flag such providers for claim review before processing so that they are not adjudicated automatically.
Public Health Role for Antibody Testing
When deciding which type of test to include in their plans, some employers are considering testing for the virus only, while others are considering testing for both the virus and antibodies.
While antibody testing results should not change risk mitigation behavior, broader antibody testing is important from a public health perspective to understand disease prevalence in the community. With further studies, the scientific evidence will eventually be able to indicate who is immune and for how long.
Who to Test and How Often?
While determining the types of testing to be used, employers must also determine their testing strategy about who to test. There are many implications to consider, including ensuring that selection of individuals to be tested is done in accordance with a prescribed process to mitigate risk of discrimination. Table 3 outlines considerations about who to test.
|
Considerations |
|
|---|---|
|
All Employees |
Logistically difficult, especially for companies with large employee populations. Costly and dependent on test and test supplies availability. |
|
Employees in Certain Roles |
Based on the industry, employees in roles where they cannot maintain physical distancing or have close interaction with customers are sometimes prioritized. |
|
Symptomatic Employees Only |
Symptomatic only has been focus of employers to date. Some companies are conducting their own testing for symptomatic employees unless those employees want to go to their own physician. |
|
High-Risk/Vulnerable Employees |
Difficult to identify. May need employee self- nomination. Local laws need to be accounted for to ensure compliance with regulations and mitigation for discrimination risk. Some laws include:
|
|
General |
|
Asymptomatic Spreaders
While most testing is focused on those who are symptomatic, it is acknowledged by health experts that 40% of the infection spread is related to asymptomatic carriers. Without testing these individuals, they pose a risk of continued spread, as other symptom- based screenings and self- isolating behavior will not apply to them. Without testing asymptomatic individuals, risk of spread continues.
Health experts say that more surveillance testing to identify infected people who are without symptoms could help contain the spread and enable a safer reopening of places like schools and businesses. To achieve this goal, health officials in the U.S. are considering a pooled testing method, where the samples of multiple people (usually 5-20) are pooled and tested as one specimen in a single test. If the test comes back negative, all people are negative. If the specimen comes back positive, follow-up individual testing is required to identify the positive case(s). Pooled testing is not new. It was first used during World War II and has subsequently been used to test for other viruses such as HIV, hepatitis. During this pandemic, city officials in Wuhan, China conducted 1.47 million tests in a single day using pooled sampling. Studies in Germany and Israel have also supported the technique’s efficacy at detecting COVID-19. "Pooling would give us the capacity to go from half a million tests per day to potentially 5 million individuals tested per day," said Dr. Deborah Birx, coordinator of the White House Coronavirus Task Force. The JAMA found that pooled sampling was more efficient and cost-effective than individual testing as long as the disease prevalence stayed under 30%.
Frequency of testing also needs to be considered. For viral detection tests such as PCR, the results only show viral status at a particular point in time. Someone could have a negative test and be exposed immediately afterward. Those in high- risk roles or consumer- facing industries may need more frequent testing. Organizations with employees directly exposed to patients with coronavirus are testing on a weekly basis. Daily testing is not clinically recommended, as it takes several days after exposure for the viral load to build up to a level that can be detected by a test.
Follow-up Actions: What to Do Following an Employee's Test results?
For symptomatic individuals who receive a negative test result, experts recommend administering a second test within 24 hours to mitigate against the risk of a false negative result. Following two negative tests, there is a greater degree of confidence that the symptoms could be due to another type of illness.
When an employee tests positive, either following employer- facilitated testing or after being notified by an employee who was tested by the health system, there are certain actions the employer needs to take, including:
Notify the employee to self- isolate at home: When an employer learns that an employee has tested positive for the virus., the employer should tell the employee to self- isolate at home and not return to the workplace until certain criteria have been met. These criteria vary based on required guidance and include:
- Later of 2 weeks and symptom- free for 3 days.
- Retesting with negative test result. Many suggest two negative test results to mitigate for risk of a false negative.
Contact tracing: Identify other colleagues with whom the employee came into contact.
- Who should be responsible for contact tracing?
- In most countries, contact tracers work for government or public health departments. Generally, contact tracing is conducted at a community level, which increases the effectiveness of the practice and ability to prevent asymptomatic, infected individuals from coming to the workplace. In the U.S., contact tracing is traditionally done by public health departments, but states, localities and employers are now quickly training contact tracers.
- Contact tracers don’t need to be medical professionals, but they do need to learn the skill of asking the right questions to determine contacts. Many employers may likely be limited in resources to perform this task. Without onsite medical personnel, the responsibility may likely fall to HR. Employers can also reach out to industry partners and local health systems to see if they have excess capacity to help do this work.
- Training: For employers embarking on contact tracing, those responsible for tracing contacts should receive some training. The CDC has contact tracing training and protocol materials that employers can use to train staff. Methodology for contact tracing includes interviewing contacts, the “manual approach,” or leveraging technology. There are advantages and disadvantages to each approach. Some countries have mandated that a single smartphone app or technology be used for the purposes of expedient contact tracing. In the U.S., there is no single technology recommended for use. Currently, for employers, the contact tracing process is a mostly manual process of interviewing employees about where they went within the workplace, including common areas like the bathroom and break rooms, and with whom they came into contact. Some employers that have cameras within their stores are using footage to increase the accuracy of determining contacts that have been made.
- Privacy is paramount: Those responsible for contact tracing on behalf of an employer must be aware of and adhere to local privacy requirements. Be careful not to disclose the identity of the employee who tested positive but notify the person (or persons) with whom that individual came into contact.
- Testing plan: If your company is facilitating testing, determine during the strategy planning phase if you will also offer testing to contacts of those employees who tested positive, or if you instead plan to refer them to community resources. People who have been in contact with someone who has a confirmed case of COVID-19 should get tested. If they test positive, the contact tracing process begins again to see who they have contacted.
While employer-led contact tracing of employees is an important mitigation strategy, it is limited to employee contacts. It does not solve for broader contact tracing needs, such as those in the community with whom employees come in contact outside of the workplace.
Notification of required health authorities: Many geographies have requirements regarding notification to government or health authorities regarding knowledge about any employees.
- Any positive COVID-19 test in the United States is reportable by the clinical laboratory or health care provider to the applicable state Department of Public Health. The public health department (or the local police department) will then generally notify employers that one of their employees tested positive (usually without divulging the name).
- Some countries that require employers to report include India, Italy and Colombia.
- Some countries prohibit an employer reporting results to the authorities: Israel. Other countries do not require or prohibit employer reporting, including Germany, Australia and the U.K.
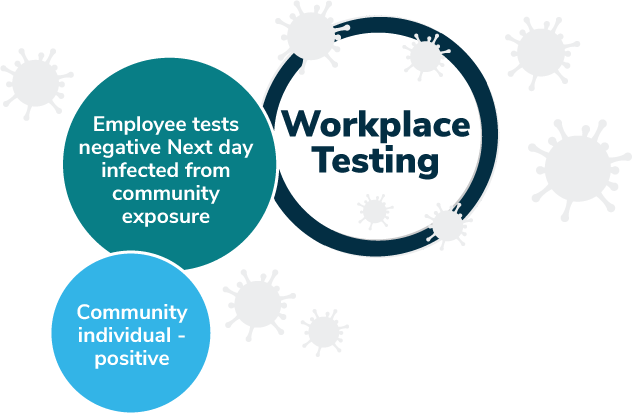
Risk Mitigation, Not Risk Elimination
No level of employer- facilitated testing will be able to eliminate the risk of exposure to the virus. During an infectious disease pandemic, mitigation needs to be addressed from the community for the best results. Employer actions cannot replace a public health response. As Figure 4 outlines, even with a robust testing plan in the workplace, employees will be exposed to community members without access to the same employer testing. As restrictions relax, more exposure and cases will ensue. Until there is a vaccine or evidence of herd immunity, risk of exposure will increase as businesses reopen. While many actions can be taken by employers to mitigate the degree of risk of reopening, many factors are outside the employers’ control. Managing employee expectations regarding risk mitigation efforts is key to addressing employee concerns about their physical and psychological safety.
More Topics
Articles & Guides-
IntroductionReturn-to-Workplace Employer Guide
-
Part 1Return-to-Workplace: Who Should Return to the Workplace and When?
-
Part 2Return-to-Workplace: Entry Screening Requirements: Symptom Checkers and Temperature Checks
-
Part 3Return-to-Workplace: Employer Strategy: To Test or Not to Test
-
Part 4Return-to-Workplace: Workplace Readiness
-
Part 5Return-to-Workplace: Employee Communications Strategies and Lessons Learned
This content is for members only. Already a member?
Login
![]()
