July 25, 2022
Many employers have prioritized mental health for some time, but the COVID-19 pandemic offered an opportunity for them to reevaluate and recommit to their mental health benefit offerings for employees and their dependents. Some revamped their Employee Assistance Programs (EAPs), and others implemented innovative mental health offerings. While important, these mental health offerings may not adequately address suicide prevention, an issue of critical and rising importance that requires specific strategies and protocols, as well as unique clinical skill sets.
This resource focuses on the need for suicide prevention among U.S. employees and family members. It also outlines the current risk of suicide and provides guidance to employers on actions they can take using the following multipronged approach:
- 1 | Reassess mental health offerings to ensure that their program and providers are equipped to identify suicide risk and qualified to assist employees and their families concerned about suicide risk or handling crisis situations.
- 2 | Maintain a workplace culture that values respect, psychological well-being and social support to reduce the incidence of predictive factors for suicidality and tackle mental health concerns among individual employees with more immediacy.
- 3 | Develop and administer trainings on crisis protocols to prepare leadership, managers and co-workers for the unfortunate occurrence of a tragedy.
Words Matter
Throughout this document, the term “died by suicide” is used rather than “committed suicide” to avoid shifting blame to the victim. The Business Group encourages all members to adopt similar terminology when discussing this issue.
Sobering Statistics on Suicide
In 2020, there were an estimated 1.2 million suicide attempts in the U.S., with over 45,000 Americans dying by suicide, averaging almost 130 suicides per day.1 Suicide is also a global issue, as over 700,000 people worldwide die from suicide every year. As a result, other high-income countries, such as South Korea, Japan, and Australia, are working to curb their high suicide rates.2, 3
Suicide is a top ten leading cause of death in the U.S. for people ages 5-64, and about 80% of all people who die by suicide are of working age (18-65).4, 5 The trend in suicides that occur in the workplace also continues to rise, with 2019 showing the highest number on record (307).6 Indirect effects of the pandemic may worsen these numbers, as certain risk factors for suicide, such as anxiety and depressive disorder, have reportedly increased by 30% in adults in the U.S. from June 2019 to January 2021.7
For people ages 10-14 and 25-34, suicide is the second leading cause of the death in the U.S., signifying that suicide risk is not only high for relatively younger members of the workforce, but also children and dependents of older working adults.4 Over 6,000 U.S. youth ages 10-24 died by suicide in 2020, and suspected suicide attempts among girls ages 12-17 increased by 51% between February and March of 2021 compared to the same period between 2019 and 2020.8 Furthermore, suicide rates in the U.S. are not impervious to disparities: The suicide rate for Black boys and men ages 15-24 increased by 47% from 2013 to 2019, and the rate for Black girls and women the same age increased by 59%.9 According to a national survey of over 33,000 LGBTQ+ youth by The Trevor Project in 2021, more than half of transgender and non-binary youth seriously considered suicide (53%), and 49% of Black youth who identify as LGBTQ+ seriously considered suicide.10
The suicide rate for veterans is among the highest in the U.S., with over 17 veteran suicides per day.11 The age- and sex-adjusted rate of veteran suicides was 26.9 per 100,000 in 2019, with veterans experiencing a suicide rate 52.3% higher than their nonveteran counterparts.11 Veterans ages 18-34 experience the highest suicide rates, at 44.4 per 100,000, a rate almost three times higher than nonveterans the same age.11, 12 These numbers show that U.S. veterans are not receiving the care they need to prevent such tragedies from happening after they return from their service. Among the average daily suicide rate of 17.2 among veterans, even those with Veterans Health Administration (VHA) encounters in 2018 or 2019 accounted for 6.8 suicides per day, meaning the help they may be receiving is not effective enough.11
Indicators from a wide range of groups point to an urgent need to address suicidality for both working-age adults and their dependents, and employers are uniquely positioned to do so. It is essential that employees and their families have access to culturally competent mental health care that addresses people's lived experiences. In recent years, companies have begun to take a more proactive role in suicide prevention, evidenced by the fact that prevention has become a higher priority within their health and well-being strategy. In addition, managers and co-workers have become more aware of how to identify risk factors and warning signs for suicide early among their colleagues.
What Is Suicidality?
Suicidality is defined by the American Psychological Association as “the risk of suicide, usually indicated by suicidal ideation or intent, especially as evident in the presence of a well-elaborated suicidal plan,” and can also be defined to include suicidal thoughts, plans, gestures or attempts.13, 14
The Emotional and Economic Toll of Suicide
Emotional Toll.
The true value of a life is immeasurable, as is the cost when one is lost. There is no way to grasp the impact of the psychological pain of those with suicidal ideation and those left behind after a suicide occurs. Grief reactions experienced by those exposed to suicide (i.e., know someone who died by suicide) can include feelings of shock, denial, anger, confusion and guilt.15, 16 Exposure to suicide and its impacts can be far-reaching and harmful, often determined by the nature of the relationship or perceived closeness to the decedent. Family, friends, colleagues and acquaintances can all be exposed to the loss and experience trauma that has the potential to last forever. Studies have found increased likelihood of suicide ideation among suicide-exposed individuals and twice the likelihood of diagnosable depression among suicide-exposed individuals compared to those not exposed to a suicide.17 Perceived closeness to the decedent not only increases the odds of depression, anxiety, and posttraumatic stress disorder, but also adds to how pervasive the after-effects of suicide can be.17 A ripple effect can ensue in the wake of a suicide, where the psychological impact on exposed individuals can influence their relationships, personality, self-worth, motivation and many other aspects of their lives.15, 16, 18 The impact of suicide on the workplace can be extremely detrimental, and morale among colleagues can sharply decline.18
Economic Toll
Beyond the emotional toll, the economic ramifications of suicide on U.S. industry are staggering. According to the Centers for Disease Control and Prevention (CDC), suicides and suicide attempts cost the U.S. almost $70 billion per year, averaging about $1.5 million per suicide in medical and work-loss costs.19 According to Greenberg and his colleagues, the economic burden of suicide among U.S. adults increased from $10.9 billion in 2010 to $13.4 billion in 2018 (year 2020 values), a 22.8% increase.20 Additionally, earnings lost due to suicide in the U.S. is an estimated $4.26 billion.21
Risk Factors, Precipitating Factors and Workplace Predictors of Suicide
Risk factors for suicide are characteristics of an individual or their environment that may predispose them to developing suicide ideation and increase the likelihood that they will die by suicide. Risk factors can vary across groups depending on age, sex, culture and other characteristics.22, 23 On the other hand, according to the Suicide Prevention Resource Center (SPRC), precipitating factors are “stressful events that can trigger a suicidal crisis in a vulnerable person.”22 While certain industries and occupations, such as mining, construction, agriculture and transportation, experience relatively more suicide-related incidents among their employees, workplace-related predictors of suicidality are varied and can impact virtually any job in any industry.24 Understanding the connection between suicidality and factors related to the workplace gives employers an opportunity to address this growing problem and provide targeted suicide prevention resources for employees and their dependents.
Table 1 presents examples of both risk and precipitating factors, as well as workplace-related predictors of suicide.
Table 1: Suicide Risk Factors, Precipitating Factors and Workplace-Related Predictors
| Risk Factors | Precipitating Factors | Workplace-Related Predictors |
|---|---|---|
|
|
|
Note: This is not an exhaustive list of all risk factors, warning signs, or workplace-related predictors.
Sources: From Suicide Prevention Resource Center. Risk and protective factors. https://www.sprc.org/about-suicide/risk-protective-factors.
From Risk and protective factors. 2021 2021/05/13/T09:20:56Z. Centers for Disease Control and Prevention. https://www.cdc.gov/suicide/factors/index.html.
From What employers need to know about suicide prevention, by K,Follme and MC Howard. Harvard Business Review. 2022.
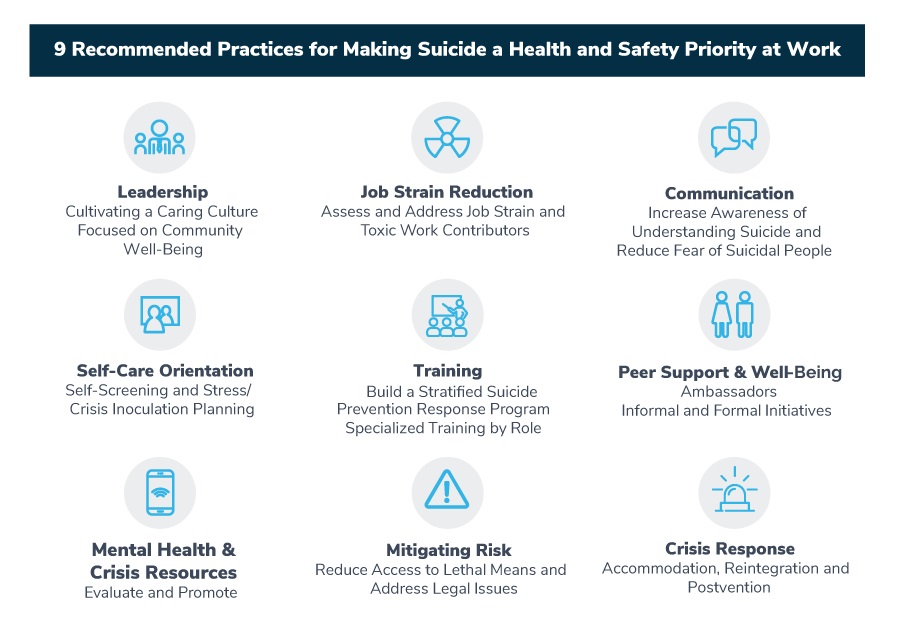
In addition to recognizing the signs of individuals potentially at risk for suicide, it is equally important to know how to address it in the workplace. Figure 1 identifies workplace practices that can be implemented to keep employees safe.
Employers Can Influence Suicide Prevention Within and Beyond the Workplace
Employers can play an important role within the wider public health framework by enhancing their suicide prevention and postvention efforts. Employees are members of many communities, and actionable steps employers take to prioritize the health of their employees can have downstream impacts on the broader population. These impacts can be especially substantial when it comes to changing cultural norms, destigmatizing suicide and mental health issues, and understanding risk factors and warning signs for suicidality. Employers can considerably decrease the incidence of suicide throughout the country with a focus on prevention, specialized care and short- and long-term postvention strategies.
What Is Postvention?
According to the SPRC, postvention is defined as “an organized response in the aftermath of a suicide to accomplish any one or more of the following:
- To facilitate the healing of individuals from the grief and distress of suicide loss;
- To mitigate other negative effects of exposure to suicide; and/or
- To prevent suicide among people who are at high risk after exposure to suicide.” 25
The Myth of Triggering Suicide Prevents Employers from Discussing Suicide Prevention
The fear of triggering suicide can inhibit beneficial and candid discussions about employee well-being, mental health resources and suicide prevention. Fear of suicide contagion also contributes to workplace reticence on the issue. Contagion refers to the phenomenon of certain types of news coverage or media that increase the likelihood of suicide among vulnerable individuals.26 While risk of contagion is more common among youth, it can be the result of a multitude of factors that push an individual to suicide. Thus, it is more likely that individuals affected by suicide contagion have been considering suicide for a long time, so raising the topic to speak about prevention is unlikely to be a contributor of a suicide.27, 28
The ability of employers and managers to change the long-term suicidal ideation exhibited by an employee is dependent upon whether they have the opportunity to intervene, at what stage they intervene and how intensely they intervene. The National Institute of Mental Health outlines a five-step action plan to help individuals in crisis:
- 1 | Ask at-risk individuals if they are thinking about suicide.
- 2 | Keep them safe by reducing their access to highly lethal items and places.
- 3 | Be there to listen to them carefully and acknowledge their feelings.
- 4 | Help them connect to the National Suicide Prevention Lifeline.
- 5 | Stay connected to them by following up and staying in touch after a crisis.
Speaking about suicide and suicide prevention resources sends a message to employees that a safe, confidential and compassionate space exists in the workplace if an employee needs it.
Key Employer Considerations for Enhancing Suicide Prevention Efforts
How do employers build a positive workplace environment? A good first step is to assess the strategies below to determine how they can be adapted to each workplace. The following section provides additional information about each approach.
Culture
- 1 | Secure buy-in from leadership to invest in suicide-prevention and postvention strategies and provide clear and repetitive messaging about the resources.
- 2 | Solidify mental health as an organizational priority by holding everyone, regardless of rank or title, especially people managers, to a standard of behavior, and promote awareness expected of the organization.
- 3 | Focus on upstream strategies for suicide prevention, including prioritizing inclusivity, diversity, equity and inclusion (DEI) initiatives and cultivating resilience among the workforce.
Benefits and Programs
- 1 | Partner with external experts to identify high-quality suicide prevention providers and counseling services and learn what outcomes are used to assess their competencies in this area.
- 2 | Turn to local resources and crisis centers when starting to build high-quality suicide prevention programs.
- 3 | Assess and understand limitations of scalable mental health products and make sure they are supplemented, if necessary, by more targeted mental health programs that include a robust suicide prevention component.
- 4 | Collaborate with existing chronic disease support vendors to make sure their programs incorporate suicide education and prevention strategies, and their nurses and counselors are trained in recognizing suicide risk.
Training
- 1 | Train HR and managers to identify and engage with at-risk individuals by not only asking questions but listening empathetically and guiding them to the resources they need. Empower them to have discussions about suicide and mental health with employees and consider implementing or mandating Mental Health First Aid training for existing and new managers.
- 2 | Communicate availability of national crisis resources, such as 988, the new three-digit dialing code for the National Suicide Prevention Hotline launched on July 16, 2022, to provide tools to deal with emergency situations in and outside the job site, in addition to showcasing your company-specific programs and vendors equipped to support suicide prevention.
- 3 | Train all staff on crisis management protocols to ensure the highest level of preparedness in the event of an employee suicide.
- 4 | Establish acute-stage, short-term and long-term response protocols and resources to support family members and co-workers touched by suicide.
Discussion of Recommendations and Strategies
Culture
Establish and Showcase Leadership Support on Suicide Prevention Strategies
The culture of an organization is set from the top down. As such, leadership can set the tone for dialogue about suicide prevention and support strategies by endorsing long-term investment in mental health benefits and suicide prevention programs. In order to influence a culture shift to normalize speaking about suicide in the workplace, clear and consistent messaging about the availability of suicide prevention resources is necessary, which also serves to showcase leadership support and organizational commitment to the issue. Alongside repetitive and visible messaging, it is important for leadership to set expectations with their human resources departments to make sure they understand the importance of letting employees talk freely about suicide prevention. By creating a space for open conversations about suicide, leaders can, in turn, encourage managers to take the initiative to openly converse with lower-level employees about suicide prevention and mental health resources. Organizational leaders championing the cause empowers managers at all levels below them and gives managers more autonomy to have discussions about mental health.
Complementary to a leader’s influence comes the need to discourage employees who are challenging the positive cultural shift. Instances may occur where certain supervisors may be reluctant or even resistant to the change of embracing open and empathetic dialogue about mental health. Leaders must play a part in elevating mental health as a priority. Identifying and educating managers whose inflexible behavior or reluctance are not conducive to this important cultural shift is necessary. Reducing this friction is another way leaders can demonstrate their commitment to the sea change in company culture.
Use Inclusivity and Culture as ’Upstream’ Suicide Prevention Strategies
Crisis management strategies and access to health care providers skilled in suicide prevention are both crucial, but prevention strategies should be implemented further upstream. Upstream elements refer to preventive strategies that can be implemented by organizations prior to the need for or use of health care services. The societal dependence on downstream activities, such as therapy, while essential, can further overwhelm providers who are either unequipped to manage in-need patients or unable to intervene in useful ways at crucial times. For example, the average wait time to see a therapist in the U.S. is 48 days, which is too long for an individual thinking about suicide.29 Employers can take actions located further upstream in the spectrum of suicide prevention strategies to challenge predictive factors of suicidality before providers, vendors and use of other health care services come into play.
Inclusivity is one such upstream element that is an inherent ally in suicide prevention strategies. During the pandemic, social connectedness gained newfound importance among employees who are both returning to in-person work and/or continuing to work remotely. The ability to collaborate with colleagues on projects and build meaningful relationships within and outside work can have direct impacts on an employee’s job satisfaction and mental well-being.18 Conversely, when acts such as bullying and harassment go unaddressed in the workplace, it can breed risk factors and/or suicide-related thoughts in at-risk employees. Promoting a company culture that prioritizes inclusivity among all different types of people and combats exclusion is a step toward emotional well-being and suicide prevention.
Creating an inclusive culture falls on leaders as well. In fact, company leadership teams that lack diversity must take the initiative to familiarize themselves with the many layers of inclusivity and its impacts. In the last few years, social justice movements have pushed companies to elevate their role in society and escalate diversity, equity, and inclusion (DEI) initiatives. These efforts, clearly connected to progress and representation in the workplace, also have a place in suicide prevention. While suicide is a leading cause of death among youth, LGBTQ+ youth (ages 13-24) are four times more likely to seriously consider suicide.30 Therefore, it is incumbent upon employers to provide a safe space for all employees, regardless of race, ethnicity, nationality, culture, religion, socioeconomic status, ability, gender identity and expression, or sexual orientation. Understanding that different perspectives and situations may come with various impacts on an employee’s mental health can allow employers to get ahead of potential mental health issues emerging among their workforce.
As previously noted, establishing an organizational culture that promotes open sharing and destigmatizes mental health issues is fundamental to suicide prevention strategies in the workplace. It is essential for employees to feel safe and reassured, and promoting psychological well-being as a company-wide priority can show dedication to these values. In doing so, employers can help their workforce build resilience, which has shown to be a protective factor against suicide risk in studies over the last 10-15 years.31 Resilience is the capacity to positively adapt in the face of risk and adversity, and it is positively correlated with psychological well-being.32 Some of the workforce support efforts implemented during the pandemic had the underlying goal of increasing employee resilience, especially important during a time when employees were juggling their personal and professional responsibilities while dealing with lockdowns and overall changes to interpersonal etiquette. Cultivating resilience among employees is another upstream suicide prevention strategy, one that concentrates on reducing the incidence of stress-related disorders but can also inhibit progression to suicidal behavior.
Benefits and Programs
Actively Seek to Include Suicide-Specialized Care in Mental Health Benefit Offerings
Offering high-quality, low-cost accessible mental health benefits is another necessity in promoting the well-being of employees and their families and a protective factor against suicide ideation.33 The Business Group’s 2022 Large Employers’ Health Care Strategy and Plan Design Survey illustrated how employers are focused on increasing access to mental health benefits for employees. However, mental health programs need to include suicide-specialized care to properly promote suicide prevention and augment care for traditional risk factors, such as anxiety, depression and trauma.8
Screening programs for suicide risk can help identify at-risk employees, but they must also connect them to follow-up care. Unfortunately, however, doing so can be a challenge. Combined with a high-quality provider network, steerage to accessible therapists can be a strong component of mental health offerings, but one in four patients report that they don’t have access to an in-network therapist.8 Developing a strong mental health provider network is essential to building a robust suicide prevention program. Many suicide prevention experts and organizations have experience assessing research-based outcomes, and employers can lean on these experts to assist with finding providers who demonstrate proficiency in treating suicidality.
Though behavioral health professionals are exposed to suicide frequently, many remain undertrained to handle treatment, as one in three have never had suicide training.8 Even among behavioral health professionals who are trained, only 61% report confidence in their ability to use evidence-based therapy to treat suicidal thoughts and behaviors.8 Measuring outcomes to evaluate treatment efficacy can help employers keep their network providers accountable. When attempting to find high-quality suicide prevention providers, employers can turn to local crisis centers as a starting point; these facilities are usually the best equipped to offer suicide prevention resources.
Experts note that EAPs are not enough to work as a stand-alone suicide prevention program and should not be treated as one. Employers can lean on products that can be scaled up to meet the mental health needs of their employees, but they must understand the limitations of these products, as they are only one component of a comprehensive mental health strategy. Scaling up effective programs specialized in suicide prevention and connecting them to existing mental health resources may be the most efficient strategy. Some employers have taken the route of implementing a suicide prevention pilot program among a targeted employee population to evaluate effectiveness, accompanied by the investment and understanding of whom it should target.
Chronic Illness, Caregivers and Suicidality
Chronic disease is categorized as a risk factor for suicide, as it is associated with a decreased quality of life that can result in psychological distress and negative impacts on work and personal relationships.34 Cancer patients in particular experience a suicide risk 1.5 times that of the general population, and those with an especially poor prognosis have 3 times the risk for suicide.34 The issue of increased suicide risk among these populations must be prioritized by utilization management programs that support cancer care, palliative care and end-of-life care.
Caregivers, or people who provide informal care to an adult with physical or mental health needs, are frequently overlooked regarding their struggles and needs.35 There are an estimated 47.9 million adult caregivers in the U.S., with an unpaid workload valued at around $470 billion every year.36 During the pandemic, among U.S. caregivers for adults who are also parents of young children, 50% reported that they had experienced serious suicidal thoughts, pointing to a desperate need for public health efforts tailored to this population.37 When considering these unseen roles and burdens employees may shoulder, companies should partner with vendors who are not only skilled in delivering medical care for chronic disease patients but are also educated on suicide prevention for these patients and their caregivers.
Evidence-based Psychosocial Interventions
Three of the most well-known, evidence-based psychosocial interventions to treat suicidality in patients are: 1) cognitive behavioral therapy (CBT), 2) dialectical behavioral therapy (DBT), and 3) the Collaborative Assessment and Management of Suicidality (CAMS) model. CBT is among the most effective psychosocial treatment for reducing suicidality in patients, as shown from randomized controlled trials (RCTs).38, 39 DBT, like CBT, can reduce and prevent onset of suicidal ideation, prevent post-treatment suicide attempts and reduce hospitalizations and emergency department (ED) visits.38, 40 Evidence from some studies suggests that CAMS is as effective in reducing suicide attempts and self-harm behaviors as DBT (Table 2).41, 42 Finding providers who have experience administering these three evidence-based practices for treating suicide is important for patients dealing with a wide range of issues related to suicide.
Table 2: A Closer Look at Suicide-Specific Evidence-Based Practices
| Methods | Treatments & Outcomes | |
|---|---|---|
| Cognitive Behavioral Therapy (CBT) |
|
|
| Dialectical Behavioral Therapy (DBT) |
|
|
| Collaborative Assessment and Management of Suicidality (CAMS) |
|
|
Sources: From Brodsky BS, Spruch-Feine, A, Stanley,B. The zero suicide model: Applying evidence-based suicide prevention practices to clinical care. Frontiers in Psychiatry. 2018; (9): 33.
From Suicide Prevention Resource Center. Cognitive therapy for suicide prevention. 2016. https://www.sprc.org/resources-programs/cognitive-therapy-suicide-prevention.
From Suicide Prevention Resource Center. Dialectical behavior therapy. 2006. https://www.sprc.org/resources-programs/dialectical-behavior-therapy.
From Brown S, et al. Embedding an evidence-based model for suicide prevention in the National Health Service: A service improvement initiative. International Journal of Environmental Research and Public Health. 2020; 17(14): 4920.
From Suicide Prevention Resource Center. Collaborative assessment and management of suicidality (CAMS). 2017. https://www.sprc.org/resources-programs/collaborative-assessment-management-suicidality-cams.
Training
Build Preparedness for Crisis Situations Through Training
Training HR professionals and managers can be especially valuable in identifying at-risk employees and guiding them to the appropriate care resources. In 2022, 75% of employers surveyed reported adoption of manager trainings to help recognize mental health issues in employees and direct them to the appropriate care.43 Training in safe messaging techniques can help employers understand how to approach typically uncomfortable conversations about suicide. Managers should be prepared to suggest resources, such as crisis hotlines, local crisis centers, available referrals and appropriate employer benefits that may have been overlooked and not utilized.44 Trainings on identifying predictive factors of suicide can help employers focus on changing negative elements within the organization and refer those showing warning signs for screening so that they can begin down the care pathway that is right for them. Organizations such as the National Council for Mental Wellbeing offer trainings, such as Mental Health First Aid, for employers looking to educate their staff on how to assist someone experiencing a crisis in a safe and responsible manner. Additionally, Workplace Suicide Prevention developed A Manager’s Guide to Suicide Postvention in the Workplace, outlining 10 action steps to deal with the aftermath of a suicide. Employers can refer to resources such as these to supplement their suicide prevention programs and improve their capability for handling these crisis situations if they arise.
Training managers can be a strong element in employer suicide prevention programs, but training all employees further solidifies the drive toward company-wide culture change. Each and every employee should know how to identify warning signs, engage with someone who may be at-risk, intervene when necessary and proceed during and after a crisis to ensure utmost preparedness throughout the organization. Among the 19 large employers surveyed in our Responding to Potential Risk of Self-Harm or Suicide in the Workplace Quick Survey, 12 employers reported that they do not conduct training on their mental health crisis protocol, and 9 employers did not know whether the team or certain individuals reach out to emergency contacts of an employee in crisis, indicating a glaring gap that could be generalized to the preparedness of many companies.45 In the event a suicide is attempted or occurs, employers need to have a plan in place to offer immediate support for affected individuals, including the employee’s family and colleagues. Training for all employees can be worthwhile for employers and HR to avoid confusion and panic if an employee experiences a crisis.
Postvention: The Acute-Stage, Short-Term and Long-Term Interventions
Postvention can include many forms of assistance that can help those impacted after a tragic event. After a suicide, exposed individuals may need psychological first aid, crisis management resources and other types of relief to cope with trauma or other negative effects and feelings. Postvention for suicide can assume several forms depending on the time period after the suicide occurs, and it is imperative to be prepared for the multiple stages after the tragedy.
In the immediate aftermath of a suicide, or the acute-stage, a plan needs to be in place for the employer to respond effectively to those exposed and offer help where it is needed. Clear and safe communication of death by suicide while respecting the privacy and dignity of people involved is necessary to avoid confusion and misleading information. Employers can work with news media to encourage safe reporting of the incident, inform essential individuals and ensure the privacy of the family or other close parties. Offering aid to family members and close co-workers who are exposed can facilitate the mourning process, and having professional or peer-support for family and colleagues can bolster treatment for those who need it.46
In the short-term period following a suicide, ongoing support should be offered to affected persons in order to effectively treat the trauma they experienced. Not all people grieve the same way, and recovery is not a linear process. Individuals may experience varying levels of grief, and they may communicate that grief differently each day on the path to healing. While managers, HR, and other leadership can encourage healthy grieving activities, they should also be attentive to forms of grieving that may manifest in numerous ways, such as divergence from typical behavior, personality changes or practices tied to their culture. Managers should give employees time and space to process their grief on their own and address their needs when seen or voiced, as a an inflexible action plan for all employees may not just be ineffective, but may also exacerbate trauma.47 Encouraging employees to take time off via paid leave can be one of the most useful and tangible elements of support that employees will appreciate. Managers and leadership can focus on a back-to-work plan, which can be therapeutic for employees needing to return to a sense of normalcy after grieving the suicide of a colleague. Allowing for mourning activities while honoring the life of the deceased and offering support resources, such as referrals to suicide survivor support groups and EAP counseling services, are critical to this stage in the postvention timeline.48
Finally, a long-term postvention strategy enlists mindfulness by employers to consider important milestones or anniversaries that may elicit emotional responses from employees exposed to the suicide. Referring to the incident with a respectful tone, honoring those who have died by suicide and continuing to offer mental health and suicide prevention resources characterize a strong long-term response. Continued investment into suicide prevention programs as a part of overall mental health offerings is needed to reduce the probability of suicide deaths in the future.18, 48 For employers that already have a prevention and postvention strategy in place, evaluation of these policies and protocols is necessary to keep them from being outdated and ineffective. A suicide prevention program must include steps to revisit these strategies regularly and make necessary updates.
Activities in Suicide Prevention on the Hill
President Biden emphasized the need for increased attention to mental health services and suicide prevention in his State of the Union on March 1, 2022. Congress is committed to using federal funding to support the initiatives via inclusion in the FY 2022 and FY 2023 budgets.
The Biden Administration released a set of goals and actions in November of 2021 to decrease the rate of suicide among the military and veteran populations. The overall strategy, fully outlined in this report, concentrates on five priority areas: 1) improve lethal means safety; 2) enhance crisis care and facilitate care transitions; 3) increase access to and delivery of effective care; 4) address upstream risk and protective factors; and 5) increase research coordination, data sharing and evaluation efforts.49 Since the release of this plan, first steps have been taken, as the Department of Veterans Affairs (VA) intends to award almost $52 million in grants for suicide prevention programs to community groups as of this past April.50
As part of the FY 2022 budget, the National Suicide Prevention Lifeline received $101.6 million to support the newly designated three-digit suicide prevention hotline, 988, which launched on July 16, 2022 nationwide.51 These funds will be used to enhance and prepare crisis centers for an expected surge in calls as they hire and train individuals to keep round-the-clock staffing, but this level of funds may not be enough to prepare for the launch as states lag behind legislation needed to implement and fund the new hotline.52, 53 The Substance Abuse and Mental Health Services Administration (SAMHSA) estimates that about $110 million is needed annually to fund the hotline’s continued operation, with an estimated $560 million needed to scale up local crisis centers in preparation for the influx of calls, but only 13 states have enacted legislation to fund the hotline despite a federal mandate.53
SAMHSA also called for the continued partnership between state and federal agencies to ensure longitudinal success of the 988 hotline. The proposed budget for FY 2023, which includes a $697 million investment into the hotline and the Behavioral Health Services Program, is a step in the right direction, but states must do more to ensure full preparedness for the launch of the hotline and its lasting efficacy.53, 54 This funding seeks to improve the National Suicide Prevention Hotline infrastructure via several avenues, including a reinforced broadband connection, improved data collection, efficient mobile crisis outreach units, increased facilitation between 988 and 911 services, assistance to call centers with minimal resources, hiring staff for follow-up services, and increased training for call center staff.54 Finally, $22 million in the proposed FY 2023 budget is dedicated to the CDC’s Comprehensive Suicide Prevention Program, which evaluates and informs suicide prevention programs across the country using the data they collect.54
With the recent enhanced focus on mental health throughout the country, these investments in mental health services and suicide prevention from the federal government may help to decrease the incidence of suicide among the working age population in the U.S. They also indicate an opportunity for employers to engage in collaborative programs with the organizations receiving these funds to support the communities where their employees live.
Conclusion
Suicide is the 12th leading cause of death in the U.S., with rising levels of depression through the pandemic adding to a growing risk of suicide. Nonetheless, 93% of adults surveyed believe suicide can be prevented at least some of the time.1, 55 While over 90% of people who die by suicide were living with a diagnosable mental health condition at the time of their death, mental health conditions often go undiagnosed or untreated.56 By implementing key considerations outlined in this article, employers can take steps to significantly impact suicide prevention. The need for comprehensive mental health benefits, including a robust suicide prevention program, can identify at-risk individuals and connect them to the appropriate care services to impede the progression to suicidal ideation from traditional risk factors. Employer efforts can make a substantial difference in not just addressing the many barriers to care patients face, but also advancing societal efforts focused on preventing future tragedies and supporting those who have been impacted by suicide in their communities.
Recommended resources to seek help if you or someone you know is having thoughts of suicide:
In the U.S.:
- U.S. National Suicide Prevention Lifeline: 988
- U.S. Crisis text line: 741741 text HOME
- The Trevor Project: For young LGBTQ+ lives
- Trans Lifeline: 877-565-8860
- Didi Hirsch Mental Health Services
Note: All calls to U.S. hotlines are free and available 24 hours a day, seven days a week. All conversations are confidential.
Outside the U.S.:
- The International Association of Suicide Prevention lists suicide hotlines by country here
- Befrienders Worldwide
- IFOTES: International Federation of Telephone Emergency Services lists helplines and emotional support centers here
- Lifeline International lists helplines by country here
More Topics
Articles & Guides
This content is for members only. Already a member?
Login
![]()
