May 01, 2019
- More employers than ever cover therapies for autism spectrum disorder (ASD), including 57% that cover applied behavioral analysis (ABA) therapy in 2018.
- Employers are beginning to implement virtual care solutions to offer support for caregivers of children with ASD, including legal counseling and resources for interacting with local school systems for class placement and other issues.
Summary of Employer Recommendations
- 1 | Consider covering ABA therapy, along with evidence-based pharmaceutical options, when making plan design decisions for treatments for ASD.
- 2 | Expand access to care through navigators and health plan partnerships.
- 3 | Communicate the availability of caregiver support services and programs to employees and spouses.
- 4 | Implement workplace policies and programs that support caregivers of children with developmental disabilities.
Background and Impact on Employees and their Families
What is ASD?
Autism Spectrum Disorder (ASD) is an umbrella term for neurodevelopmental disorders, such as autistic disorder and Asperger syndrome, that were previously diagnosed separately.1 ASD is characterized by difficulties with social interaction, limits in communication and language and repetitive behaviors, although the symptoms can be different for each child. ASD is often accompanied by other conditions, including a seizure disorder, mental retardation, hyperactivity and anxiety.2
The causes of ASD are unclear and likely involve many factors, including genetics. Extensive research has shown that vaccines are not a cause of ASD.3 ASD generally requires chronic management over the lifespan.
The American Academy of Pediatrics recommends that all children be screened for ASD between the ages of 18 and 24 months, along with regular developmental surveillance.4 The Centers for Disease Control and Prevention (CDC) estimates that the prevalence of ASD was one in 59 among children aged 8 years old in the United States with some variation across sex, race/ethnicity, and geography.5 Children with ASD tend to have higher health care costs and require a higher level of support from their caregivers.
Health Care Costs for Children with Autism
Individuals with ASD have average medical expenditures that exceed those without ASD by anywhere from $4,110 to $6,200 per year.6 Furthermore, an analysis of the Medical Expenditure Panel Survey (MEPS) found that children with ASD had a higher annual mean number of clinic visits compared with children in the control group (5.6 vs 2.8 visits per year).7 Average costs across the board were higher for children with ASD: hospitalizations among children with ASD in a group health plan were $550 compared to $208 per year for those without ASD; clinic visits were $1,373 compared to $540 per year; and prescription medications were $724 compared to $96 per year.8sup> Non-medical expenses associated with raising a child with ASD are estimated at more than $14,000 per year, including $8,610 higher in education costs alone.9
Caregivers for Dependents with Special Needs
Parents of children with special needs have higher rates of anxiety and depression than other parents, with the highest rates among those who have children with ASD.10,11 In fact, 46% of caregivers of children with special needs report that they need more help or information managing their emotional/physical stress, and 40% said they need more help or information balancing work/family responsibilities.12
Providing care for any dependent with special needs is also associated with increased absenteeism and work limitations.10 One study found that mothers of children with a developmental delay or disability lose approximately five hours of work weekly, totaling approximately 250 hours per year.13 The demands of caring for a child with ASD can often force a parent to leave the workforce.
Treatment Options for ASD
Medications
There are no drugs currently approved to treat ASD’s core symptoms, which include communication difficulties, social challenges and repetitive behavior.14 However, a range of medications are used to treat individuals with ASD, including but not limited to antipsychotics, antidepressants, and stimulants. Many of these medications are used to treat co-morbid symptoms of ASD (hyperactivity, depression/anxiety, irritability and severe challenging behavior) and are often prescribed off-label. Risperidone and aripiprazole are approved for addressing irritability associated with ASD.
Complementary and alternative medicine (CAM) interventions
While complementary interventions include those in the medical sphere, such as diets and the use of supplements, these treatments tend to focus on symptoms and associated difficulties like touch aversion. Allied health interventions may include occupational and language and physical therapy, while CAM interventions may include acupuncture and massage.14
ABA Therapy
ABA is an umbrella term describing principles and techniques used in the assessment, treatment and prevention of challenging behaviors and the promotion of new desired meaningful behaviors. The goal of ABA is to teach new skills, promote generalization of these skills, and reduce challenging behaviors with systematic reinforcement. The principles and techniques of ABA existed for decades prior to specific application and study within ASDs. ABA may be delivered by different providers in a variety of settings, formats, and levels of intensity including the following:
- Comprehensive treatment packages;
- High intensity 1-on-1 treatments for many hours a week by para/professionals;
- Parent training formats;
- Social skills interventions; or
- Embedded within allied health and educational interventions such as feeding therapy or classroom instruction.
Allied health and educational interventions can focus on honing communication/language, social, adaptive behaviors, and learning/academic skills as well as address challenging behaviors (e.g. self-injury, aggression, elopement, noncompliance, etc.). ABA is often packaged with other treatments and relies heavily on positive reinforcement to modify behavior.
Limits on Benefits for ABA Therapies
A 2018 Business Group survey found that 73% of large employer respondents do not place limits on ABA benefits. For those who do have limits, the most common type was on age (17%), which ranged from 12 to 26 years old. Among employers that limit coverage by number of visits (12%), some determined the limits by hours per month, as well as overall number of visits per year.
Tiered-service delivery models are often a standard part of ABA coverage strategy. Often with these models, a supervising clinician (usually Board-Certified Behavior Analyst (BCBA or BCBA-D) or psychologist) guides treatment programs for clients and oversees care delivered by para-professionals (e.g. registered behavior technicians). Such models increase the likelihood that patients get access to appropriate care given the intensity of service delivery required and availability of supervising clinicians.
Educational and learning programs
The goal of these programs is to improve educational and cognitive skills. Educational services are provided at no charge to children with disabilities, including those with ASD, through the Individuals with Disabilities Education Act (IDEA), a federally mandated program. These services may include transportation, counseling, recreation and enrichment programs, school nurse services, and physical and occupational speech therapy.17
Common educational interventions employ TEACCH, or the Treatment and Education of Autistic and Related Communication Handicapped Children model.14 Some interventions implemented in educational settings are based on principles of ABA and may be intensive. model.14
Mental Health Parity Considerations on Limitations
Employers should consider the requirements of the Mental Health Parity Act of 1996 (MHPA) and the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA). MHPA states that a plan’s (or insurer’s) annual or lifetime dollar limits on mental health benefits—including autism treatment benefits—can be no lower than the annual or lifetime dollar limits for medical and surgical benefits.
MHPAEA expanded on MHPA and stipulates that a plan’s financial requirement (e.g., deductible, copayment, coinsurance or out-of-pocket maximum) or treatment limitation (e.g., limit on frequency of treatment, number of visits or days of coverage) for mental health or substance use disorder benefits can be no more restrictive than the “predominant” financial requirement or treatment limitation that applies to “substantially all” medical and surgical benefits. This translates in the following ways with respect to autism treatment coverage:
- If a financial requirement (such as a copayment) or treatment limitation (such as a visit limit) does not apply to at least two-thirds of all medical and surgical benefits in a classification (such as outpatient, in-network), then that financial requirement or treatment limitation cannot be applied to outpatient, in- network autism treatment benefits.
- A plan cannot have separate cumulative financial requirements or treatment limitations for mental health or substance use disorder benefits in the same classification. For example, a plan cannot have a 50-visit limit for medical and surgical visits and a separate 50-visit limit for autism treatment. However, a combined 50-visit limit for medical/surgical, mental health and substance use disorder benefits would be permissible.
- The MHPAEA also requires parity with respect to non-quantitative treatment limits, such as preauthorization requirements and residential treatment limits. For example, a plan must ensure that any limit to residential treatment for substance use disorders applies no more stringently to the majority of all
Employer Approaches to Covering Treatments for ASDs
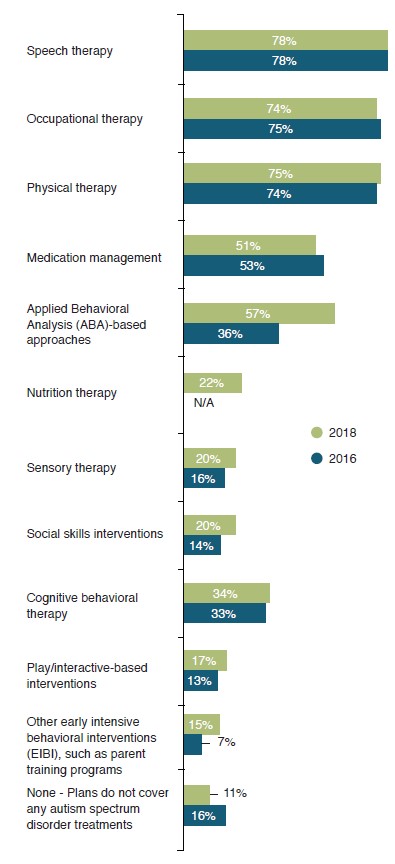
In 2018, 89% of large employers cover at least some type of treatment commonly used for children with ASD (see Figure 1).20 While speech, occupational and physical therapy remain the most commonly covered services, other interventions are notably increasing in prevalence of coverage.16 In particular, 57% of employers now cover ABA (up from 36% in 2016), and 15% cover
Considering Eligibility Limits
Employers covering treatments for autism need to consider whether they will place limits on coverage for these services, such as a cap on the number of hours per week (quantitative limit) or a requirement that the treatment plan be submitted to the insurance company (non- quantitative limit). Employers should consult with their legal counsel to make sure these limits are compliant with mental health parity regulations.
Supports for Caregivers of Dependents with ASDs
Employers can support parents of children with autism in several ways:
- Implement flexible work schedules, reduced work time and telecommuting options for parents;
- Contract with a vendors that provide educational services and supports for parents of children with ASD;
- Provide access to respite care, either through an on-site provider, standalone facilities or in the home;
- Connect parents to ASD-specific health plan care managers and employee assistance program (EAP) providers, who can help coordinate care and navigate families through the health care system;
- Ensure that accommodations are made for children with developmental disabilities to enable them to participate in employer events such as “Bring Your Child to Work Day”; and
- Provide financial counseling specifically for parents of children with ASD, which may include the creation of trusts to support them.
Source: National Business Group on Health. Large Employers’ 2018 Health Care Strategy and Plan Design Survey.
As understanding of ASD, its impact on functioning, and the number of treatment options continue to grow, more research is needed to address the following:13
- Early markers of treatment success and the techniques of multicomponent therapies that drive effectiveness;
- More information on which children are most likely to benefit from treatment;
- Which treatment approaches to use in children under age 2 at high risk for developing autism; and
- Whether there is any harm associated with behavioral, educational, allied health or complementary and alternative medicine interventions.
Many treatments used by families with children with ASD have insufficient evidence to determine whether they are effective or not. These include:
- Medications like serotonin reuptake inhibitors, omega-3 fatty acids and hyperbaric oxygen; and
- Other complementary or alternative treatments like music therapy and weighted blankets.
Employer Recommendations
Consider available evidence when making coverage decisions for treatments for autism.
Where evidence is clear that a treatment is effective or harmful, employers should align their coverage decisions with the evidence. This includes:
- Consideration of coverage for ABA therapy, which has been shown to be effective when targeted for early intensive treatment. Ask your health plan and consultant partners for data on utilization and cost of this therapy across their book of business. Consider requiring pre-authorization for ABA therapy, and steering those using the therapy to Board Certified Behavioral Analysts to ensure that providers adhere to ABA practice guidelines.
- Coverage for risperidone and aripiprazole (brand names Risperdal® and Abilify®, respectively) in your prescription drug formulary.
- Exclusion of secretin and chelation products from coverage for ASD. In addition to the finding that these drugs are not effective at improving autism symptoms, the FDA reports there are serious safety issues associated with chelation products, including dehydration, kidney failure and death.13
Expand access to care through navigators and health plan partnership.
Gaps in provider networks for specialists, such as speech language pathologists, psychiatrists, psychologists and audiologists are an unfortunate reality across the country.
- Ask your health plans about available autism navigator services under your plan and work together to communicate this service to parents of children with autism. Consider virtual care options available.
- Ask your health plan about credentialing requirements for network providers. Some services, like ABA, can be effectively delivered by lower-level practitioners (e.g., practical nurses, aides, BCaBAs) less expensively and to a greater patient population. Consider requiring ABA therapy certification as a condition of coverage.
Communicate the availability of autism support services to employees and spouses.
Coverage of evidence-based treatment, restrictions in place and available programs to support parents should be communicated clearly and in a targeted way to families with children with ASD.
Personalized, proactive outreach by third-party vendors should be considered to:
- Educate parents of children diagnosed with ASD on available resources, including case management or other navigator services, that can help parents choose providers, coordinate care and facilitate collaboration with providers outside the health care team.
- Consider contracting with third-party vendors that provide parental education services specifically for autism. Health plans and EAPs should direct parents to these services once they’re identified as eligible participants.
- Provide decision-support information on ASD treatments that includes types of treatments and specialists; treatment goals and realistic expectations; and the side effects and potential harms of treatments.
Implement workplace policies and programs that support caregivers of children with autism.
- Provide information on caregiving and the risk of depression to employees who apply for Family Medical Leave (FML) and make available depression screening with a standardized instrument (e.g., PHQ-9 or PHQ-2). FML programs should refer employees who screen positive for depression to appropriate behavioral health specialists or the EAP.
- Provide employees with information on local or online support groups. Alternatively, if there is enough demand at a work site, sponsor a location-specific support group for parents of children with ASD. Workplace events that encourage attendance by families with children with ASD or special needs can increase awareness, boost camaraderie and create an opportunity for further communication of resources available for parents.
- Consider providing coverage for respite care providers, who can look after children with autism while caregivers have time to rest and address other basic day-to-day responsibilities.
- Allow for flexible or reduced work schedules and telecommuting for parents of children with ASD.
Summary
There is a growing body of evidence to guide treatment choices for ASD, including some encouraging results on early intensive behavioral interventions. However, there are still significant gaps in knowledge about the comparative effectiveness of treatments and which children populations are likely to benefit from which interventions. Virtual care point solutions and concierge services can provide individual assessments to help prepare children with ASD for school, along with supplemental guidance on early interventions. In addition, employers can use existing health, decision support, case management and EAP programs to help parents of children with ASD make provider and treatment choices for their children and themselves.
Additional Resources
More Topics
Articles & Guides- 1 | Autism Speaks. DSM-5 and Autism: frequently asked questions. http://www.autismspeaks.org/dsm-5/ faq. Accessed August 28, 2018.
- 2 | Autism Treatment Trust, Treating Autism. Medical comorbidities in autism spectrum disorders. Accessed November 17, 2016.
- 3 | Centers for Disease Control and Prevention. Concerns about autism. https://www.cdc.gov/vaccinesafety/concerns/autism.html. Accessed August 28, 2018.
- 4 | American Academy of Pediatrics. Autism initiatives. https://www.aap.org/en-us/advocacy-and-policy/aap- health-initiatives/Pages/autism-initiatives.aspx. Accessed October 23, 2018.
- 5 | Centers for Disease Control and Prevention. Autism spectrum disorder (ASD) – data & statistics. https:// www.cdc.gov/ncbddd/autism/data.html. Accessed August 14, 2018.
- 6 | Shimabukuro TT, Grosse SD, Rice C. Medical expenditures for children with autism spectrum disorder in a privately insured population. J Autism Dev Disord. 2008;38(3):546-552.
- 7 | Lavell T, et al. Economic Burden of Childhood Autism Spectrum Disorders. Pediatrics. 2014;133(3):e520-e529.
- 8 | Croen LA, et al. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. em>Pediatrics. 2006;118(4):e1203-e1211.
- 9 |Lavelle TA, et al. Economic burden of childhood autism spectrum disorders. em>Pediatrics. 2014;133(3):e520-e529.
- 10 | Burton WN, et al. Caregiving for ill dependents and its association with employee health risks and productivity. J Occup Environ Med. 2004;46(10):1048-1056.
- 11 | Hamlyn-Wright S, Draghi-Lorenz R, Ellis J. Locus of control fails to mediate between stress and anxiety and depression in parents of children with a developmental disorder. Autism. 2007;11(6):489-501
- 12 | National Alliance for Caregiving. AARP. Caregivers of children: a focused look at those caring for a child with special needs under the age of 18. http://www.caregiving.org/pdf/research/Report_Caregivers_of_Children_11-12-09.pdf. 2009. Accessed August 28, 2014.
- 13 | Powers ET. Children’s health and maternal work activity: estimates under alternative disability definitions. J Hum Resou. 2004;38(3):522-556.
- 14 | Warren Z, et. al. Therapies for children with autism spectrum disorders. Comparative Effectiveness Review No. 26, Rockville, MD: Publication No. 11-EHC029-EF. April 2011.
- 15 | Autism Speaks. Medicines for treating Autism’s core symptoms. https://www.autismspeaks.org/what- autism/treatment/medicines-treating-core-symptoms. Accessed August 14, 2018.
- 16 | . National Business Group on Health. Autism spectrum disorder benefits. Accessed September 27, 2017.
- 17 | Autism Speaks. Applied behavior analysis (ABA). https://www.autismspeaks.org/applied-behavior-analysis-aba-0. Accessed October 23, 2018.
- 18 | Behavior Analyst Certification Board. Applied behavior analysis treatment of autism spectrum disorder: practice guidelines for healthcare funders and managers. https://www.bacb.com/wp-content/ uploads/2017/09/ABA_Guidelines_for_ASD.pdf. Accessed on October 23, 2018.
- 19 | Carolina Coast Behavioral Services. Tiered service delivery model. http://www.ccbs-sc.com/index.php/ aboutustop/abatherapy/14-sample-data-articles/97-tieredservice. Accessed on October 23, 2018.
- 20 | National Business Group on Health. Large employers’ 2018 health care strategy and plan design survey. Accessed August 15, 2018.
This content is for members only. Already a member?
Login
![]()
